Abstract
We have analysed retrospectively the influence of different sources of knee deformity on failure of closing wedge high tibial valgus osteotomy (HTO). Preoperative frontal plane varus deformities of the lower extremity, distal femur and proximal tibia, and medial convergence of the knee joint line were assessed on a standard whole leg radiograph in 76 patients. Using the logistic regression model, the probability of survival for HTO was 77% (SD 4%) at 10-years follow-up. Varus deformity of the lower extremity (< 175°), and medial convergence of the knee joint line (> 3°) were identified as preoperative risk factors for conversion to arthroplasty (P = 0.03 and P = 0.006). We found no evidence that varus inclination of the proximal tibia or distal femur influences long-term survival of HTO.
Similar content being viewed by others
Introduction
High tibial valgus osteotomy (HTO) is a well accepted treatment of medial unicompartmental osteoarthritis of the knee with varus alignment in active patients. Results, however, seem to deteriorate in time, and this group of patients may ultimately require knee replacement [16]. One of the key factors for long-term HTO success is the achievement of an even distribution of the mechanical load of the knee joint by obtaining an ideal lower-extremity mechanical axis alignment. This may be influenced by preoperative axial alignment parameters such as the tibiofemoral angle, which has been found to predict conversion to arthroplasty and patient dissatisfaction [5]. Also, preoperative varus deformity of the distal femur has been observed to be associated with varus recurrence and poor results 7 years after HTO [15]. On the other hand, patients with specific anatomical conditions such as congenital bowing of the proximal tibia have been reported to benefit more from a valgus correction osteotomy than patients with varus of the proximal tibia caused by degenerative changes [1]. The Lyon knee school postulated that valgus correction of a constitutional tibia varus deformity restores tibia alignment in a curative way, and thus creates a more physiological knee load distribution [7]. Therefore, Bonnin and Chambat suggested measuring the “tibial bone varus angle” according to Lévigne to help differentiate between a bony deformity of the proximal tibia and secondary bony erosion, with a worse prognosis [1, 7].
The objective of the present study was to analyse the influence of different sources of knee varus deformity on failure of closing wedge HTO at 10-year follow-up. Failure was defined as conversion to total knee arthroplasty (TKA), because avoiding knee replacement is one of the main reasons to perform HTO. First, we determined preoperative axial alignment parameters in a group of patients who underwent closing wedge HTO because of symptomatic medial unicompartmental knee osteoarthritis. Then, we investigated the relation between failure of HTO and different sources of knee varus deformity in the frontal plane.
Materials and methods
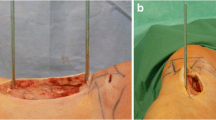
We used a cohort of 114 patients who had 122 lateral closing wedge HTOs, performed between 1991 and 1997 because of symptomatic medial osteoarthritis. A closing wedge technique through a transverse incision with the patient in supine position was performed in all patients. Subsequently, the anterior part of the proximal tibia-fibular syndesmosis was resected. Under fluoroscopic guidance, we used a calibrated slotted wedge resection guide of Allopro (Zimmer; Winterthur, Switzerland) to remove the wedge proximal to the patellar tendon insertion. The size of the wedge was determined preoperative using the medial Hip-Knee-Ankle (HKA) angle measured from a standardized whole leg radiograph (WLR). The goal was to achieve a correction of 4° in excess of neutral alignment [10]. The osteotomy was fixated with two-step staples. All patients were mobilized on the first postoperative day, and partial weight-bearing in a standard cylinder plaster cast was allowed for 6 weeks.
Before surgery, a WLR in standing position was performed in all patients. The patient stood barefooted on the affected leg with the knee in full extension, while the contra-lateral flexed knee was supported by means of a small box. The X-ray beam was centred on the affected knee with the tube at a distance of 1.5 m. The three-part 136/36-cm cassette with graduated grid was immediately behind the patient. The 100% anteroposterior projection was ensured during lateral fluoroscopic control by superimposing the dorsal aspect of the femoral condyles. The tube was set perpendicular to this lateral view and was moved from the proximal end to the distal end so that a WLR was obtained. We retrieved 90 preoperative WLRs; of which five patients with post-traumatic bone deformities, one patient with total hip replacement, and one patient with rickets were excluded for analysis. The baseline characteristics for the included 76 patients with 83 osteotomies (7 patients with staged bilateral procedures) are shown in Table 1; we found no significant differences between the study population and 31 patients with 32 osteotomies (1 patient with staged bilateral procedure) who had irretrievable WLRs. Failure of the osteotomy was defined as the need for conversion of HTO to a TKA. Patients records were reviewed, and patients or relatives of the patients who had died, were interviewed via telephone to obtain the postoperative status at the time of follow-up. The average time of follow-up was 12 years (range 10–17 years). Nineteen osteotomies (23%) were revised to a TKA at the 10-year follow-up. The average time between the osteotomy and TKA was 6.2 (SD 2.6) years. Three patients had died from an unrelated condition 3, 8, and 10 years after the osteotomy. In none of these patients the osteotomy had been converted to a TKA.
Measurements
In 83 knees the medial HKA angle was measured, and defined as the medial angle between two lines: one line of the centre of the femur head using Mose circles to the top of the femoral notch (mechanical axis line of the femur), and a second line from the centre of the ankle to the centre of the tibial spines (mechanical axis line of the tibia) (Fig. 1). The lateral distal femoral angle (LDFA) was determined to measure distal femoral bone alignment, and defined as the lateral angle formed between the mechanical axis line of the femur and the knee joint line of the femur (Fig. 2) [12]. Proximal tibia varus deformity was determined by the medial proximal tibia angle (MPTA). MPTA was defined as the medial angle between the knee joint line of the tibia and the mechanical axis line of the tibia (Fig. 3) [12]. The tibial bone varus angle (TBVA), which does not measure possible bone or cartilage loss of the medial tibia plateau, was used to determine constitutional tibia varus deformity. TBVA was defined as the angle between a line from the centre of the tibial spines to a point midway the proximal tibia epiphysis, and the mechanical axis line of the tibia (Fig. 4) [1]. A positive value represented a varus direction of the angle described. Finally, the knee joint line convergence angle (JLCA) was assessed to determine the angle between the femoral and tibial frontal plane joint lines (Fig. 5) [12]. A positive value represented a medially converged knee joint line.
Two observers (T.R. and I.T.) measured all described angles using a manual goniometer graduated in degrees, without knowledge of clinical outcome to assess inter-observer reproducibility. The radiographs were re-measured by the same observers at least 2 weeks later, without knowledge of the results of the first readings, to assess intraobserver reproducibility. One observer (T.R.) was orthopaedic surgeon and experienced with reviewing WLR. The other observer (I.T.) was a physician attending the Orthopaedic Department. An explanation and a copy of Paley’s malalignment test and Bonnin’s paper were given as references to each observer [1, 12].
Malalignment
We considered the lower extremity varus malaligned when the HKA angle measured less than 175° [12]. When the LDFA was more than 90° the femur contributed to varus deformity, and when the MPTA angle was less than 85° the proximal tibia was a source of the varus deformity [12]. We defined constitutional tibia varus malalignment when the TBVA angle measured more than 5° [1]. JLCA was considered malaligned when the knee joint line converged more than 3°. This may be attributed to medial cartilage loss, and we also investigated the relationship (Spearman’s rho correlation) between JLCA and preoperative Ahlbäck grade [12].
Statistical analysis
The SPSS statistical software version 14.0 (SPSS Inc., Chicago, Illinois) was used for statistical analysis and a P value of 0.05 was considered to be statistically significant. The intra- and inter-observer reproducibility was assessed by two-way mixed effect model, consistency definition, and expressed as intraclass correlation coefficients (ICC) that vary from zero (no agreement at all) to 1 (total agreement). We investigated the relation between conversion of HTO to TKA and preoperative malalignment, respectively, varus deformity of the lower extremity (medial HKA angle < 175°), distal femur (LDFA > 90°) and proximal tibia (MPTA < 85° and TBVA > 5°), and medial convergence of the knee joint line (JLCA > 3°). We calculated odds ratios, by logistic regression analysis, to estimate the relation between failure of the osteotomy and preoperative frontal alignment factors. We performed multivariate, stepwise (backward) logistic regression and entered variables with a P value of ≤ 0.05 into the model. The data for this investigation were collected and analysed in compliance with the procedures and policies set forth by the Helsinki Declaration.
Results
The mean pre-HTO HKA angle of the 76 patients with 83 osteotomies was 173.1° (SD 4.1°). The mean pre-HTO distal femur alignment was in valgus with a mean of 89.1° (SD 2.4°). Pre-osteotomy proximal tibia alignment determined with the use of MPTA and TBVA measured a mean angle of 85.4° (SD 2.7°) and 6.7° (SD 4.4°), respectively. The mean pre-HTO joint line converged medially with a JLCA of 3.4° (SD 2.2°), and a positive relationship (rho = 0.3; P = 0.006) between JLCA and preoperative Ahlbäck grade of OA was found. The intra- and inter-observer agreements were excellent for HKA (ICC’s of 0.94, 0.95), and good for MPTA (ICC’s of 0.84, 0.88) and LDFA (ICC’s of 0.79, 0.75). JLCA assessment showed reasonable intra and inter-observer agreement (ICC’s of 0.69, 0.70). However, determination of TBVA had poor intra- and inter-observer agreement (ICC’s of 0.52, 0.48). The probability of survival for HTO was 77% (SD 4%) at 10-year follow-up. Using the logistic regression model, HKA angle < 175° and JLCA > 3° were identified as preoperative risk factors for conversion to arthroplasty (P = 0.03 and P = 0.006). There was a four times (95% CI; 1.2–13.3) higher chance of conversion to arthroplasty for patients with preoperative HKA < 175°, and a six times (95% CI; 1.7–24.3) higher risk for knee replacement in patients with a preoperative JLCA > 3°. Preoperative frontal plane varus deformity of distal femur (LDFA > 90°), or the proximal tibia (MPTA < 85° and TBVA > 5°) showed no significant relationship with HTO failure after 10 years (Table 2).
Discussion
Careful operative technique, adequate correction, but most of all proper patient selection seem to predict long-term outcomes of HTO. Anatomical conditions that determine knee deformity in the frontal plane have been described to influence the success of valgus correction osteotomy [1, 5, 15]. We used a historic cohort of patients who had undergone lateral closing wedge osteotomy for symptomatic medial osteoarthritis to determine the role of preoperative axial parameters of varus alignment in the failure of HTO. Although the indication and technique were standardized in our clinic, the present study was not prospective. Indicated for operation were only patients with knee motion more than 90° and with less of 15° of flexion contraction, without collateral laxity greater than the expected from the diminished joint space on physical examination, and with a medial HKA angle no less than 165°. Our analysis was limited that no knee scores or radiographs were used to measure knee function or varus deformity at the time of follow-up. The outcomes were merely based on failure of the surgical procedure. However, we considered TKA to be a clear end-point for HTO failure because avoiding knee replacement is one of the main reasons to perform HTO. Another limitation of this study was that we were able to retrieve 74% of all radiographs at 10 year follow-up. Nonetheless, we noted no significant baseline differences for the group of patients who had irretrievable images compared to the study group (Table 1). In a population with symptomatic knee osteoarthritis, knee function impairment may lead to large changes in projected angles when simultaneous flexion and rotation occur [3]. We used standing WLR with lateral fluoroscopy to ensure 100% anteroposterior projection. Earlier, we reported high intra- and inter-observer agreement of the measurement of the HKA angle with the use of this radiological technique [2]. This study demonstrated also good agreement for the measurement of MPTA (0.84; 0.88) and LDFA (0.79; 0.75), and reasonable agreement for JLCA (0.69; 0.70).
The influence of lower extremity varus deformity on outcome after HTO remains under debate. A preoperative tibiofemoral angle > 9° has been described as a predictor of HTO failure and patient dissatisfaction after HTO [5]. Another recent analysis, however, found no influence of the preoperative angle [4]. In both studies, the determination of the cut-off angles was not well specified. We defined the lower extremity varus malaligned when the medial HKA angle measured less than 175° [12], and found a significant relation between HKA angle < 175° and conversion to TKA after 10 years. Varus alignment correlates significantly with knee adduction moment [9], and Prodromos et al. [13] reported that patients with low preoperative knee adductor moments had substantially better clinical results after HTO than patients with high knee adduction moments. Another explanation might be that the HKA angle correlates well with the grade of medial compartment osteoarthritis [2]. Advanced stages of osteoarthritis have been reported to increase the revision rate of osteotomy [11]. In our clinic, we did not use preoperative stress views, but patients with collateral laxity greater than the expected from the diminished joint space on physical examination were not eligible for osteotomy. That probably explains the significant (P = 0.006) correlation we observed between JLCA converging medially and preoperative Ahlbäck grade of OA. Therefore, the size of the medial converged JLCA measured on a standing WLR, most likely represents the amount of medial joint space narrowing due to loss of medial cartilage. Spahn et al. [14] demonstrated that a medial joint space width less than 5 mm and tibial exophytes, or severe chondral damage of the medial tibia plateau predict a poor result after HTO. This study also showed that JLCA > 3° was a strong predictor of HTO failure. In a retrospective analysis of 29 patients (37 osteotomies) who underwent HTO because of medial osteoarthritis, preoperative varus inclination of the distal femur was significantly associated with poor results after a mean follow-up of 7.4 years. The authors argued that assessing the preoperative slope of the distal femur was important because it may predict recurrence of varus deformity [15]. Recurrent varus has been reported to increase the risk of HTO revision by re-osteotomy or arthroplasty [11]. Our series of 83 osteotomies was limited, in that no varus deformity was measured at the time of follow-up. The mean preoperative LDFA, however, was in mild valgus (89.1°) which suggests that excessive tilt of the joint surface after tibial osteotomy is not likely to be expected. This may explain that we did not identify preoperative distal femur varus inclination as a risk factor for HTO conversion to TKA after 10 years.
Tibia deformation is mainly due to both constitutional deformation and degenerative changes, and some have suggested that favourable candidates for HTO include patients who have proximal bowing of the tibia [1, 8]. In a series of 217 patients who underwent lateral closing wedge HTO because of symptomatic medial osteoarthritis, clinical results seemed to be better with increased bowing at 6 years follow-up [1]. Constitutional bowing is hard to distinguish from degenerative bone deformity with standard measurement techniques that assess the tibial plateaus. TBVA measurement with the use of the proximal growth cartilage scar has been proposed to determine constitutional deformity of the proximal tibia [1]. This may be helpful because possible bone loss of the medial tibia plateau will not be measured. However, when assessing TBVA on WLR, we found poor intraobserver reproducibility (r = 0.52) and unacceptable low agreement between the two observers (r = 0.48), mainly due to uncertain identification of the old epiphyseal growth plate. Jenny et al. also reported low inter-observer agreement (r = 0.41) for defining the morphology of the proximal tibia with the use of this method [6]. TBVA assessment, therefore, seems not a reliable method, and MPTA measurement may be more suitable to recognize constitutional tibia bone deformity in patients with low grade OA. In this study, the majority of patients (92%) had medial compartment OA less than Grade 3 using the Ahlbäck scoring system of knee osteoarthritis, which radiological indicates no bone loss of the proximal tibia. We considered MPTA < 85° constitutional bowing of proximal tibia [12], but found no significant relationship with HTO failure after 10 years.
In summary, we found that lower extremity varus deformity and medial convergence of the knee joint line predict failure of closing wedge HTO after a 10-year follow-up. In contrast, we found no evidence that varus bowing of the proximal tibia or distal femur influences long-term survival of HTO.
References
Bonnin M, Chambat P (2004) Current status of valgus angle, tibial head closing wedge osteotomy in medial gonarthrosis. Orthopaede 33:135–142
Brouwer RW, Jakma TSC, Bierma-Zeinstra SMA, Ginai AZ, Verhaar JAN (2003) The whole leg radiograph: standing versus supine for determining axial alignment. Acta Orthop Scand 74:565–568
Brouwer RW, Jakma TS, Brouwer KH, Verhaar JA (2007) Pitfalls in determining knee alignment: a radiographic cadaver study. J Knee Surg 20:210–215
Flecher X, Parratte S, Aubaniac J-M, Argenson J-NA (2006) A 12–28-year follow-up study of closing wedge high tibial osteotomy. Clin Orthop Relat Res 452:91–96
Huang T, Tseng K, Chen W, Lin RM, Wu J, Chen T (2005) Preoperative tibiofemoral angle predicts survival of proximal tibia osteotomy. Clin Orthop Relat Res 432:188–195
Jenny J-Y, Boéri C, Ballonzoli L, Meyer N (2005) Difficulties and reproducibility of radiological measurement of the proximal tibial axis according to Lévigne. Rev Chir Orthop Reparatrice Appar Mot 91:658–663
Lévigne C, Bonnin M (1991) Ostéotomie tibiale de valgisation pour AFTI. Journées Lyonnaises de Chirurgie du Genou, Lyon
Lootvoet L, Massinon A, Rossillion R, Himmer O, Lambert K, Ghosez JP (1993) Upper tibial osteotomy for gonarthrosis in genu varum. Apropos of a series of 193 cases reviewed 6 to 10 years later. Rev Chir Orthop 79:375–384
Miyazaki T, Wada M, Kawahara H, Sato M, Baba H, Shimada S (2002) Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Ann Rheum Dis 61:617–622
Myrnerts R (1980) High tibial osteotomy with overcorrection of varus malalignment in medial gonarthrosis. Acta Orthop Scand 51:557–560
Odenbring S, Egund N, Knutson K, Lindstrand A, Toksvig Larsen S (1990) Revision after osteotomy for gonartrosis. A 10–19-year follow-up of 314 cases. Acta Orthop Scand 61:128–130
Paley D (2003) Malalignment and malorientation in the frontal plane. In: Paley D, Herzenberg JE (eds) Principles of deformity correction. Springer, New York, pp 19–30 (Corr. 2nd printing)
Prodromos CC, Andriacchi TP, Galante JO (1985) A relationship between gait and clinical changes following high tibial osteotomy. J Bone Joint Surg 67-A:1188–1194
Spahn G, Kirschbaum S, Kahl E (2006) Factors that influence high tibial osteotomy results in patients with medial gonarthritis: a score to predict results. Osteoarthritis Cartilage 14:190–195
Terauchi M, Shirakura K, Katayama M, Higuchi H, Takagishi K, Kimura M (2002) Varus inclination of the distal femur and high tibial osteotomy. J Bone Joint Surg 84-B:223–226
Virolainen P, Aro HT (2004) High tibial osteotomy for the treatment of osteoarthritis of the knee: a review of the literature and a meta-analysis of follow-up studies. Arch Orthop Trauma Surg 124:258–261
Acknowledgment
We thank Dr R. W. Brouwer for his contributions to the manuscript.
Conflict of interest statement
The authors declare that they have no conflict of interest.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
van Raaij, T.M., Takacs, I., Reijman, M. et al. Varus inclination of the proximal tibia or the distal femur does not influence high tibial osteotomy outcome. Knee Surg Sports Traumatol Arthrosc 17, 390–395 (2009). https://doi.org/10.1007/s00167-008-0708-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-008-0708-6