Abstract
Purpose
One-fourth of the patients with exudative age-related macular degeneration (AMD) treated with an autologous retinal pigment epithelium (RPE)-choroid translocation had a hyperfluorescent optic disc with indocyanine green angiography (ICGA). This study aimed to identify whether indocyanine green (ICG)-assisted surgery was related to the hyperfluorescence of the optic disc with ICGA.
Methods
Retrospective observational case series of 31 AMD patients treated with an RPE-choroid translocation and who had ICGA after surgery. The ICGAs were assessed for hypo/iso/hyperfluorescence of the optic disc and fluorescence was related to the time interval between ICGA and the possible use of intravitreal ICG.
Results
The optic disc was hyperfluorescent in six patients, isofluorescent in one, and hypofluorescent in 24 patients. All hyperfluorescent optic discs and 7 of the 24 hypofluorescent optic discs were preceded with ICG-assisted surgery with a time interval of 7±3 weeks and 43±12 weeks, respectively (P=0.001, Student t-test). The other 17 hypofluorescent discs were not preceded by ICG-assisted surgery and the one isofluorescent optic disc was observed 32 weeks after ICG-assisted surgery.
Conclusion
There was a statistically significant correlation between intravitreal ICG use during surgery and a hyperfluorescent optic disc with ICGA in our patient group.
Similar content being viewed by others
Introduction
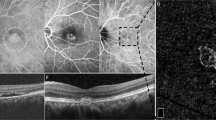
One of the first principles one learns when interpreting indocyanine green angiography (ICGA) is that the optic disc is hypofluorescent in a normal angiogram. While evaluating postoperative angiograms of patients with exudative age-related macular degeneration (AMD) treated with an autologous retinal pigment epithelium (RPE)-choroid translocation, we encountered hyperfluorescent optic discs in one-fourth of these patients (Figure 1). We initially thought of an inflammatory cause, but this was highly unlikely as clinical signs for inflammation were absent, and the time interval between surgery and ICGA was too extended in most of the patients to be a plausible cause for postoperative inflammation. Another explanation could be the prolonged staining of the optic disc after intravitreal indocyanine green (ICG) administration during posterior segment surgery to visualize the inner limiting membrane (ILM). Weinberger et al1 first reported this in 2001. The diffusion of ICG in the optic tract was subsequently described and histological confirmed by Paques et al2 in an animal model.
This report aimed to identify whether ICG-assisted surgery was related to the hyperfluorescence of the optic disc in our patients and to study its persistence.
Patients and methods
Thirty-one patients with exudative AMD treated with an RPE-choroid graft translocation and who had ICGA after surgery to exclude a possible recurrent neovascular membrane, were included in this retrospective observational case series. ICGA was performed according to a routine standard protocol in all patients.
In this surgery, initial surgery with the autologous RPE-choroid graft translocation (surgery was performed as previously described by van Meurs and van den Biesen3) is followed by silicone oil removal after 3–4 months, at which time ICG-assisted ILM removal is performed in selected patients. In two patients, the ICGAs were obtained before and in 29 patients, after silicone oil removal. The ICGAs were assessed for hypo/iso/hyperfluorescence of the optic disc and related to the time interval between ICGA and the possible use of intravitreal ICG.
Results
The optic disc was hyperfluorescent in six patients, isofluorescent in one, and hypofluorescent in 24 patients (Table 1). All ICGAs with hyperfluorescent and 7 of the 24 hypofluorescent optic discs were preceded with ICG-assisted surgery with a time interval of 7±3 weeks and 43±12 weeks, respectively (P=0.001, Student t-test). The other 17 hypofluorescent discs were not preceded by ICG-assisted surgery and the one isofluorescent optic disc was observed 32 weeks after ICG-assisted ILM peeling (Table 1).
Of the six patients with hyperfluorescent optic discs, the optic discs of both the fellow eyes (available in three patients) and operated eyes before surgery (available in five patients) were hypofluorescent.
Discussion
A causal connection between intravitreal ICG use during surgery and a hyperfluorescent optic disc with ICGA in our patient group was suggested by the statistically significant correlation and the documented neurophilic staining properties of ICG.2 Hyperfluorescence could be observed at least the first 4 months after surgery and subsequently faded away till the normal hypofluorescence was returned after about 10 months.
There are only a few articles reporting on the phenomenon of a hyperfluorescent optic disc after intravitreal ICG application and all but one have a short-term follow-up. Shortly after ICG application, hyperfluorescence of distinct areas of the retina was observed, which progressively migrated towards the optic disc with finally only the optic disc being hyperfluorescent. In these studies, hyperfluorescence of the optic disc also started to fade after about 3–6 months after surgery but could persist up to 6–12 months.4, 5, 6, 7 Only one study recently reported on the long-term follow-up (16–36 months after surgery) in 18 patients and their results suggested that ICG might even persist for years.8 An explanation for this is that they used a high-contrast sensitivity scanning laser ophthalmoscope (HRA), which is more sensitive than ICG angiography with a conventional fundus camera used in this and several other studies, because there is a lower level of light scatter.8, 9
In conclusion, since the introduction of intravitreal ICG-assisted surgery, a hyperfluorescent optic disc with ICGA may be observed more often in daily practice, a phenomenon we found to be unknown even under experienced medical retinal specialists. Therefore, if doctors see a hyperfluorescent disc in someone who recently had vitreoretinal surgery, they should ask the surgeon whether intravitreal ICG was used, rather than immediately starting a prolonged series of expensive investigations to identify an inflammatory cause.
References
Weinberger AW, Kirchhof B, Mazinani BE, Schrage NF . Persistent indocyanine green (ICG) fluorescence 6 weeks after ICG administration for macular hole surgery. Graefes Arch Clin Exp Ophthalmol 2001; 239: 388–390.
Paques M, Genevois O, Régnier A, Tadayoni R, Sercombe R, Gaudric A et al. Axon-tracing properties of indocyanine green. Arch Ophthalmol 2003; 121: 367–370.
Van Meurs JC, van den Biesen PR . Autologous retinal pigment epithelium and choroid translocation in patients with exudative age-related macular degeneration: short-term follow-up. Am J Ophthalmol 2003; 136: 688–695.
Kroemer I, Lommatzsch A, Pauleikhoff D . Retinal ICG accumulation after ILM staining during macular hole surgery? Ophthalmologe 2004; 101: 604–607.
Tadayoni R, Paques M, Girmens JF, Massin P, Gaudric A . Persistence of fundus fluorescence after use of indocyanine green for macular surgery. Ophthalmol 2003; 110: 604–608.
Sayanagi K, Ikuno Y, Soga K, Sawa M, Oshima Y, Kamei M et al. Residual indocyanine green fluorescence pattern after vitrectomy for idiopathic macular hole with internal limiting membrane peeling. Br J Ophthalmol 2007; 91: 939–944.
Machida S, Fujiwara T, Gotoh T . Observation of the ocular fundud by an infra-red-sensitive video camera after vitreoretinal surgery assisted by indocyanine green. Retina 2003; 23: 183–191.
Sekiryu T, Iida T . Long-term observation of fundus infrared fluorescence after indocyanine green-assisted vitrectomy. Retina 2007; 27: 190–197.
Flower RW, Csaky KG, Murphy RP . Disparity between fundus camera and scanning laser ophthalmoscope indocyanine green imaging of retinal pigment epithelium detachments. Retina 1998; 18: 260–268.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have no commercial or financial interest in this publication
Financial support: the SWOO-Flieringa Foundation (Foundation Scientific Research Eye Hospital Rotterdam), the Rotterdam Eye Hospital, Rotterdam, The Netherlands
Rights and permissions
About this article
Cite this article
Maaijwee, K., van den Biesen, P. & van Meurs, J. Hyperfluorescence of the optic disc with indocyanine green angiography. Eye 23, 819–821 (2009). https://doi.org/10.1038/eye.2008.146
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2008.146