-
PDF
- Split View
-
Views
-
Cite
Cite
B. J. Noordman, B. P. L. Wijnhoven, S. M. Lagarde, K. Biermann, A. van der Gaast, M. C. W. Spaander, R. Valkema, J. J. B. van Lanschot, Active surveillance in clinically complete responders after neoadjuvant chemoradiotherapy for esophageal or junctional cancer, Diseases of the Esophagus, Volume 30, Issue 12, December 2017, Pages 1–8, https://doi.org/10.1093/dote/dox100
Close - Share Icon Share
Summary
Neoadjuvant chemoradiotherapy (nCRT) followed by surgery is standard of care for locally advanced esophageal cancer in many countries. After nCRT up to one third of all patients have a pathologically complete response in the resection specimen, posing an ethical imperative to reconsider the necessity of standard surgery in all operable patients after nCRT. An active surveillance strategy following nCRT, in which patients are subjected to frequent clinical investigations after the completion of neoadjuvant therapy, has been evaluated in other types of cancer with promising results. In esophageal cancer, both patients who are cured by neoadjuvant therapy alone as well as patients with subclinical disseminated disease at the time of completion of neoadjuvant therapy may benefit from such an organ sparing approach. Active surveillance is currently applied in selected patients with esophageal cancer who refuse surgery or are medically unfit for major surgery after completion of nCRT, but this strategy is not (yet) adopted as an alternative to standard surgery or definitive chemoradiation. The available literature is scarce, but suggests that long-term oncological outcomes after active surveillance are noninferior compared to standard surgical resection, providing justification for comparison of both treatments in a phase III trial. This review gives an overview of the current knowledge regarding active surveillance after completion of nCRT in esophageal cancer and outlines future research perspectives.
INTRODUCTION
Surgical resection has long been considered the primary curative treatment modality for stages cT1b-4aN0–3M0 esophageal or junctional cancer. In the literature reported 5-year survival rates for patients treated with primary surgical resection range from six to 50%, but rarely exceed 35%.1–5 To improve long-term survival, many trials investigated the added value of neoadjuvant chemo- and/or radiotherapy. 6–12
In most countries, two neoadjuvant approaches have been adopted as standard of care. The first is neoadjuvant chemoradiotherapy (nCRT), now generally based on the CROSS regimen, which resulted in a 5-year overall survival benefit of 14%, compared to surgery alone.10,11 An alternative option is perioperative or preoperative chemotherapy using the OEO2 or the MAGIC protocol, which showed an absolute risk reduction of 6% and 13% at 5-years, respectively.7,12 Except for Japan, it is widely accepted that chemoradiotherapy is the neoadjuvant treatment of choice for patients with squamous cell carcinoma. For patients with adenocarcinoma, the optimal multimodality regimen is still topic of debate.13–15 A significant survival benefit of nCRT over nCT has never been proven for patients with adenocarcinoma, but nCRT is associated with a high percentage of pathologically complete response (pCR) for both histological subtypes.13,16,17 A pCR means that no viable tumor cells can be detected at the site of the primary tumor or in the resected regional lymph nodes, as determined by conventional histological examination.
In subsequent analyses of secondary endpoints of the CROSS trial it was found that nearly a third (29%) of the patients had a pathologically complete response (pCR) in the resection specimen. In the CROSS trial, a pCR after nCRT was seen in 49% of patients with a squamous cell carcinoma and 23% of patients with an adenocarcinoma. In the OEO2 and MAGIC trials this was 4% and 5%, respectively.10,18 This observation raises the question whether a surgical resection is of benefit for patients who were already cured locoregionally by nCRT alone. Theoretically, an organ sparing approach might be feasible since, intuitively, an esophagectomy in patients with no residual viable tumor cells has no effect on clinical outcome. An esophagectomy is associated with a risk for per- and postoperative mortality and morbidity and reduces quality of life in both the short and long term.19–24 This imposes an ethical imperative to reconsider the necessity of standard esophagectomy in patients after nCRT. An individualized approach to surgery after nCRT should be studied and defined; a new treatment algorithm in which not every patient with potentially curable esophageal cancer needs a resection after completion of nCRT to achieve long-term survival. Such an active surveillance strategy is currently applied in selected patients who refuse surgery or are medically unfit for major surgery after completion of nCRT.25–28 In this review, we give an overview of the feasibility and effectiveness of an active surveillance approach after completion of nCRT for carcinoma of the esophagus.
Rationale for an active surveillance approach
In an active surveillance strategy, patients are subjected to serial clinical investigations after completion of nCRT. Surgical resection will be offered only to patients in whom a locoregional regrowth/residual disease is highly suspected or proven, without signs of distant dissemination.
In other types of cancer including rectal and head and neck cancer, similar approaches have been evaluated with excellent results.29–32 In a recent study in patients who received nCRT for rectal cancer, 65% of all patients with a clinically complete response (cCR, i.e. no residual disease based on clinical diagnostics) did not need surgery. Of the remaining 35%, a successful delayed surgical resection was performed in 90% of patients. Oncological outcome was comparable between both treatment groups.30 In advanced head and neck cancer, active surveillance after chemoradiotherapy is widely accepted nowadays. In a recent randomized controlled trial (RCT) that compared standard neck dissection with PET-CT guided surveillance, survival was similar for both groups, but surveillance resulted in considerably fewer operations and was more cost-effective.32
Who will benefit from an active surveillance approach?
An organ-preserving active surveillance strategy in esophageal cancer will not only have advantages for individuals who are already cured by neoadjuvant therapy alone, but also for patients with subclinical disseminated disease (i.e. micrometastases) at the time of completion of neoadjuvant therapy. After tumor staging and neoadjuvant treatment, micrometastases may be present but yet undetectable. With time these disseminated tumor cells will become clinically manifest. Distant metastases, which are the main determinants of long-term survival after nCRT plus surgery (especially in patients with a pathologically complete response), are grossly independent of locoregional therapy.7,33 Although the biology of distant dissemination is not fully understood, current assumptions hold that the process of spreading and seeding of tumor cells from the primary lesion is an early event. The process of tumor cell dissemination may well have occurred at the time of first clinical presentation and subsequent locoregional treatment (i.e. nCRT with and without subsequent surgery).34 This is reflected by the large number of patients who develop hematogenous metastases within two years after surgery.10,11,35 Hence, no matter how timely and aggressive locoregional treatment is, it will hardly affect the survival-determining events of distant dissemination. At present, patients with occult distant metastases undergo an esophageal resection, which ultimately is of no benefit to them, because distant metastases are still below the detection limit at the first clinical evaluation after nCRT. It should be noted that another theoretical explanation for the high rate of distant dissemination early after esophagectomy is that the depression of the immune system after major surgery might enhance hematogenic diffusion of tumor cells. This phenomenon will not take place if the patient is not operated on.36 This hypothesis also supports an active surveillance strategy. Hence, it is hypothesized that application of an active surveillance strategy in patients with a clinically complete response after nCRT may reduce the need for an esophagectomy in 30 to 40% of all patients.10,11,25,27,28
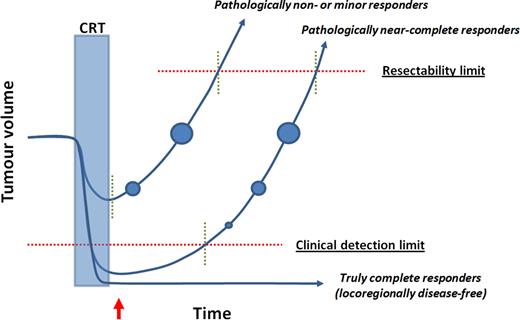
An active surveillance approach is only justified if long-term oncological outcome is similar to that after nCRT followed by surgery. Therefore, tumor regrowth after nCRT should be detected at a curable stage, i.e. in the period between the clinical detection limit* and the resectability limit and before the potential development of distant dissemination from disease regrowth (Fig. 1). Currently, the time span of this period and its variation between patients is unknown. Therefore, an intensive surveillance strategy (or approach) should be applied aiming to detect regrowth of cancer as early as possible before the tumor is irresectable. Since the majority of locoregional regrowths are expected to occur within 12 months after nCRT and nearly all within 24 months, an intensive surveillance strategy should be performed in the first two years.37
Tumor response after neoadjuvant chemoradiotherapy. CRT: chemoradiotherapy; Red arrow: time of clinical response evaluation (CRE); Vertical interrupted green lines: boundaries of theoretical time windows. First vertical interrupted green line on each curve refers to the first moment after CRT that a tumor becomes clinically detectable. Second vertical interrupted green line on each curve refers to the moment that a tumor becomes irresectable (T4b). Circles depict progression of locoregional tumor volume. The clinical detection limit is the minimal amount of disease that can be detected by the combination of symptoms, endoscopy with biopsies and imaging modalities.
Clinical response evaluations: identifying and excluding minor- and nonresponders
After completion of nCRT, all patients should be re-staged, which is defined as the clinical response evaluation (CRE). After a CRE, patients can be categorized as clinically complete responders or clinically incomplete responders. Only clinically complete responders (i.e. patients in whom no locoregional or disseminated disease can be proven) are offered active surveillance. Clinically incomplete responders with locoregional disease in the absence of distant metastases will be referred for immediate surgery, whereas clinically incomplete responders with distant metastases will be referred for palliative care or second line chemotherapy.
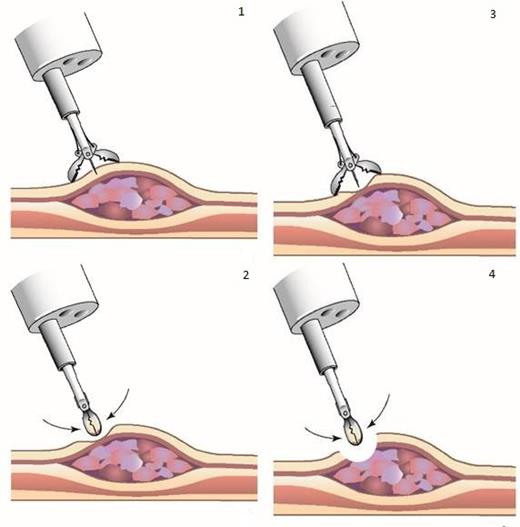
Multiple studies have focused on the accuracy of detecting residual disease during clinical response evaluation after nCRT for esophageal cancer. A surgical resection as standard treatment in a potentially curative setting was (almost) always performed. Although the accuracy of endoscopy with standard biopsies is limited (false negative rate 41%–69%),38–40 a recent study suggested that endoscopy with deep (bite-on-bite) biopsies is more accurate in detecting residual disease after nCRT. Tumor-negative bite-on-bite biopsies were 85% predictive for a pathologically complete response in the resection specimen (i.e. 15% false negative for any residual cancer).41 Bite-on-bite biopsies increase the chance of detecting residual submucosal tumor deposits compared to conventional biopsies (Fig. 2). After nCRT, residual disease is frequently located in the submucosa (and mucosa), and is rarely present as an isolated remnant only in the proper muscle layer, surrounding stroma and/or regional lymph nodes.42 The use of fine needle aspiration (FNA) to detect lymph node metastases theoretically further increases the diagnostic accuracy, but literature regarding this topic is lacking.
Bite-on-bite biopsies (1 + 2 + 3 + 4) supposedly increase the chance of detecting submucosal tumor deposits compared to conventional biopsies (1 + 2).
18F-FDG PET-CT can identify non-complete responders with moderate sensitivity (46–88%) and specificity (56–87%) during CREs. The substantial false negative (12–54%) and false positive rates (13–44%) of a single PET-CT after nCRT limit its applicability for detection of locoregional residual disease during CRE.43–48 However, PET-CT is highly valuable in the detection of interval metastases, as development of metastatic disease during the nCRT period can be detected by PET-CT in up to 10% of all patients.49 Moreover, serial PET-CT during active surveillance might be useful in the detection of local regrowths, as a subtle increase in FDG-avidity may indicate recurrence of malignancy, whereas a decrease in FDG-avidity more likely depicts the recovery from earlier radiotherapy induced esophagitis.
The maximum tumor thickness (MTT) and changes in MTT as determined by endoscopic ultrasound (EUS) are predictive for histopathological response on nCRT, as shown by a Swiss study.50 However, these findings need validation in an independent cohort.50
At present, the Dutch preSANO trial investigates the accuracy of clinical response evaluation and the optimal diagnostic set for detecting residual disease after nCRT for esophageal cancer using a combination of endoscopy with bite-on-bite biopsies, radial EUS for measurement of maximal tumor thickness and–area, linear EUS-guided FNA of suspected lymph nodes, and 18F-FDG PET-CT.51 Approximately six weeks after completion of nCRT, a first CRE is performed including endoscopy with bite-on-bite biopsies and EUS. Patients in whom no residual disease can be proven by histology will be offered postponed surgery, approximately 12–14 weeks after completion of nCRT. One week before the planned surgical resection, a second clinical response evaluation (CRE-II) is performed with a PET-CT scan followed by endoscopy with bite-on-bite biopsies, EUS and FNA of all suspected lymph nodes and/or PET-positive lesions. The rationale to include this second CRE is to increase the absolute chance of detecting residual disease and to allow for a comparison between serial measurements. The safety of delaying surgery to 12–14 weeks is supported by a recent study suggesting that prolonged time to surgery after nCRT up to at least 12 weeks has no negative effect on disease-free and overall survival (HR = 1.00 and HR = 1.06 per additional week). Moreover, prolonged time to surgery increases the probability of a pathologically complete response in the resection specimen (odds ratio = 1.35 per additional week of time to surgery, P= 0.0004).52 Similar results have been published by other groups.53–55 The main study parameter of the preSANO trial is the correlation between clinical response during the CREs and pathological response in the resection specimen. Results of the preSANO trial are expected end-2017 and will reveal the optimal combination of diagnostic tests to detect residual disease after nCRT.51
Although several studies have investigated the accuracy of detecting residual disease after nCRT, the minimum accuracy needed for testing an active surveillance strategy in a clinical trial is under debate. Intuitively, any residual disease after nCRT may not be missed since these patients do not benefit from active surveillance and should undergo surgery as soon as possible. On the other hand, as long as tumor regrowth after nCRT can be detected at a curable stage during active surveillance (Fig. 1), long-term oncological outcome is theoretically not jeopardized and residual disease may be missed during initial CREs. This conception is supported by the available literature on active surveillance after nCRT for rectal or esophageal cancer, which shows that a delayed (radical) resection can be performed successfully in nearly all patients with locoregional regrowth that was detected during active surveillance using endoscopy with (conventional) biopsies and PET-CT (see below).25,27,28,30 It should be noted that a postponed surgical resection has been suggested to increase the risk of postoperative complications. However, this phenomenon is reported mainly after treatment with high dose of definitive chemoradiotherapy (radiotherapy dose >50 Gy; so called salvage esophagectomy) in low-volume centers and it is unknown whether this also applies after treatment with a lower dose of radiotherapy (CROSS regimen).56,57 Taken together, it is felt that the decision to perform a phase III trial that compares active surveillance with standard surgery should not depend on a predefined minimum sensitivity or negative predictive value of response evaluation, but rather on results from (phase I/II) studies that have reported clinical outcomes of an active surveillance strategy in selected patients with a cCR after nCRT. Nevertheless, results from studies on diagnostic accuracy are highly valuable, especially for determination of the optimal composition of a diagnostic set of tests for response and surveillance evaluations.
Outcomes after active surveillance: a systematic review
A systematic review was conducted to provide a complete overview of all literature on clinical outcomes of active surveillance after nCRT.
Methods
A systematic literature search on active surveillance after neoadjuvant chemoradiotherapy for esophageal cancer was performed in Embase, Medline Ovid, Web of Science, Scopus, and the Cochrane Library databases from the inception of the databases to August 9th 2016 by using the search terms ‘esophageal cancer,’ ‘active surveillance’ and ‘neoadjuvant chemoradiotherapy’ and its synonyms in the title and abstract fields (Table 1). The literature search was performed by an independent specialized literature researcher. Two reviewers independently screened titles and abstracts of the retrieved publications.
Search strategy for systematic review on clinical outcomes after active surveillance
| Database . | Search . | Hits . |
|---|---|---|
| Embase | (‘esophagus cancer’/exp OR ‘esophagus tumor’/de OR (((esophag* OR oesophag*) NEAR/6 (cancer* OR neoplas* OR carcino* OR adenocarcino* OR tumor* OR tumour* OR malign*))): ab, ti) AND (‘watchful waiting’/de OR (((watch* OR see) NEAR/3 wait*) OR (active* NEAR/3 surveil*) OR ((selective* OR reserv* OR selected* OR needed OR necessar* OR unnecessar* OR declin* OR avoid* OR on-demand) NEAR/6 (resect* OR surg* OR resect* OR esophagectom* OR oesophagectom*))): ab, ti) AND (‘chemoradiotherapy’/exp OR (chemoradi* OR radiochemo* OR (chemotherap* NEAR/6 radiotherap*)): ab, ti) | 284 |
| Medline Orvid | (‘Esophageal Neoplasms’/OR (((esophag* OR oesophag*) ADJ6 (cancer* OR neoplas* OR carcino* OR adenocarcino* OR tumor* OR tumour* OR malign*))).ab, ti.) AND (‘Watchful Waiting’/OR (((watch* OR see) ADJ3 wait*) OR (active* ADJ3 surveil*) OR ((selective* OR needed OR necessar* OR unnecessar* OR declin* OR avoid* OR on-demand) ADJ6 (resect* OR surg* OR resect* OR esophagectom* OR oesophagectom*))).ab, ti.) AND (exp ‘Chemoradiotherapy’/OR (‘Chemotherapy, Adjuvant’/AND ‘Radiotherapy, Adjuvant’/) OR (chemoradi* OR radiochemo* OR (chemotherap* ADJ6 radiotherap*)).ab, ti.) | 106 |
| Cochrane | ((((esophag* OR oesophag*) NEAR/6 (cancer* OR neoplas* OR carcino* OR adenocarcino* OR tumor* OR tumour* OR malign*))): ab, ti) AND ((((watch* OR see) NEAR/3 wait*) OR (active* NEAR/3 surveil*) OR ((selective* OR needed OR necessar* OR unnecessar* OR declin* OR avoid* OR on-demand) NEAR/6 (resect* OR surg* OR resect* OR esophagectom* OR oesophagectom*))): ab, ti) AND ((chemoradi* OR radiochemo* OR (chemotherap* NEAR/6 radiotherap*)): ab, ti) | 110 |
| Web of science | TS = (((((esophag* OR oesophag*) NEAR/5 (cancer* OR neoplas* OR carcino* OR adenocarcino* OR tumor* OR tumour* OR malign*)))) AND ((((watch* OR see) NEAR/2 wait*) OR (active* NEAR/2 surveil*) OR ((selective* OR needed OR necessar* OR unnecessar* OR declin* OR avoid* OR on-demand) NEAR/5 (resect* OR surg* OR resect* OR esophagectom* OR oesophagectom*)))) AND ((chemoradi* OR radiochemo* OR (chemotherap* NEAR/5 radiotherap*)))) | 248 |
| Scopus | TITLE-ABS-KEY(((((esophag* OR oesophag*) W/5 (cancer* OR neoplas* OR carcino* OR adenocarcino* OR tumor* OR tumour* OR malign*)))) AND ((((watch* OR see) W/2 wait*) OR (active* W/2 surveil*) OR ((selective* OR needed OR necessar* OR unnecessar* OR declin* OR avoid* OR on-demand) W/2 (resect* OR surg* OR resect* OR esophagectom* OR oesophagectom*)))) AND ((chemoradi* OR radiochemo* OR (chemotherap* W/5 radiotherap*)))) | 5 |
| Total | 753 | |
| Database . | Search . | Hits . |
|---|---|---|
| Embase | (‘esophagus cancer’/exp OR ‘esophagus tumor’/de OR (((esophag* OR oesophag*) NEAR/6 (cancer* OR neoplas* OR carcino* OR adenocarcino* OR tumor* OR tumour* OR malign*))): ab, ti) AND (‘watchful waiting’/de OR (((watch* OR see) NEAR/3 wait*) OR (active* NEAR/3 surveil*) OR ((selective* OR reserv* OR selected* OR needed OR necessar* OR unnecessar* OR declin* OR avoid* OR on-demand) NEAR/6 (resect* OR surg* OR resect* OR esophagectom* OR oesophagectom*))): ab, ti) AND (‘chemoradiotherapy’/exp OR (chemoradi* OR radiochemo* OR (chemotherap* NEAR/6 radiotherap*)): ab, ti) | 284 |
| Medline Orvid | (‘Esophageal Neoplasms’/OR (((esophag* OR oesophag*) ADJ6 (cancer* OR neoplas* OR carcino* OR adenocarcino* OR tumor* OR tumour* OR malign*))).ab, ti.) AND (‘Watchful Waiting’/OR (((watch* OR see) ADJ3 wait*) OR (active* ADJ3 surveil*) OR ((selective* OR needed OR necessar* OR unnecessar* OR declin* OR avoid* OR on-demand) ADJ6 (resect* OR surg* OR resect* OR esophagectom* OR oesophagectom*))).ab, ti.) AND (exp ‘Chemoradiotherapy’/OR (‘Chemotherapy, Adjuvant’/AND ‘Radiotherapy, Adjuvant’/) OR (chemoradi* OR radiochemo* OR (chemotherap* ADJ6 radiotherap*)).ab, ti.) | 106 |
| Cochrane | ((((esophag* OR oesophag*) NEAR/6 (cancer* OR neoplas* OR carcino* OR adenocarcino* OR tumor* OR tumour* OR malign*))): ab, ti) AND ((((watch* OR see) NEAR/3 wait*) OR (active* NEAR/3 surveil*) OR ((selective* OR needed OR necessar* OR unnecessar* OR declin* OR avoid* OR on-demand) NEAR/6 (resect* OR surg* OR resect* OR esophagectom* OR oesophagectom*))): ab, ti) AND ((chemoradi* OR radiochemo* OR (chemotherap* NEAR/6 radiotherap*)): ab, ti) | 110 |
| Web of science | TS = (((((esophag* OR oesophag*) NEAR/5 (cancer* OR neoplas* OR carcino* OR adenocarcino* OR tumor* OR tumour* OR malign*)))) AND ((((watch* OR see) NEAR/2 wait*) OR (active* NEAR/2 surveil*) OR ((selective* OR needed OR necessar* OR unnecessar* OR declin* OR avoid* OR on-demand) NEAR/5 (resect* OR surg* OR resect* OR esophagectom* OR oesophagectom*)))) AND ((chemoradi* OR radiochemo* OR (chemotherap* NEAR/5 radiotherap*)))) | 248 |
| Scopus | TITLE-ABS-KEY(((((esophag* OR oesophag*) W/5 (cancer* OR neoplas* OR carcino* OR adenocarcino* OR tumor* OR tumour* OR malign*)))) AND ((((watch* OR see) W/2 wait*) OR (active* W/2 surveil*) OR ((selective* OR needed OR necessar* OR unnecessar* OR declin* OR avoid* OR on-demand) W/2 (resect* OR surg* OR resect* OR esophagectom* OR oesophagectom*)))) AND ((chemoradi* OR radiochemo* OR (chemotherap* W/5 radiotherap*)))) | 5 |
| Total | 753 | |
Search strategy for systematic review on clinical outcomes after active surveillance
| Database . | Search . | Hits . |
|---|---|---|
| Embase | (‘esophagus cancer’/exp OR ‘esophagus tumor’/de OR (((esophag* OR oesophag*) NEAR/6 (cancer* OR neoplas* OR carcino* OR adenocarcino* OR tumor* OR tumour* OR malign*))): ab, ti) AND (‘watchful waiting’/de OR (((watch* OR see) NEAR/3 wait*) OR (active* NEAR/3 surveil*) OR ((selective* OR reserv* OR selected* OR needed OR necessar* OR unnecessar* OR declin* OR avoid* OR on-demand) NEAR/6 (resect* OR surg* OR resect* OR esophagectom* OR oesophagectom*))): ab, ti) AND (‘chemoradiotherapy’/exp OR (chemoradi* OR radiochemo* OR (chemotherap* NEAR/6 radiotherap*)): ab, ti) | 284 |
| Medline Orvid | (‘Esophageal Neoplasms’/OR (((esophag* OR oesophag*) ADJ6 (cancer* OR neoplas* OR carcino* OR adenocarcino* OR tumor* OR tumour* OR malign*))).ab, ti.) AND (‘Watchful Waiting’/OR (((watch* OR see) ADJ3 wait*) OR (active* ADJ3 surveil*) OR ((selective* OR needed OR necessar* OR unnecessar* OR declin* OR avoid* OR on-demand) ADJ6 (resect* OR surg* OR resect* OR esophagectom* OR oesophagectom*))).ab, ti.) AND (exp ‘Chemoradiotherapy’/OR (‘Chemotherapy, Adjuvant’/AND ‘Radiotherapy, Adjuvant’/) OR (chemoradi* OR radiochemo* OR (chemotherap* ADJ6 radiotherap*)).ab, ti.) | 106 |
| Cochrane | ((((esophag* OR oesophag*) NEAR/6 (cancer* OR neoplas* OR carcino* OR adenocarcino* OR tumor* OR tumour* OR malign*))): ab, ti) AND ((((watch* OR see) NEAR/3 wait*) OR (active* NEAR/3 surveil*) OR ((selective* OR needed OR necessar* OR unnecessar* OR declin* OR avoid* OR on-demand) NEAR/6 (resect* OR surg* OR resect* OR esophagectom* OR oesophagectom*))): ab, ti) AND ((chemoradi* OR radiochemo* OR (chemotherap* NEAR/6 radiotherap*)): ab, ti) | 110 |
| Web of science | TS = (((((esophag* OR oesophag*) NEAR/5 (cancer* OR neoplas* OR carcino* OR adenocarcino* OR tumor* OR tumour* OR malign*)))) AND ((((watch* OR see) NEAR/2 wait*) OR (active* NEAR/2 surveil*) OR ((selective* OR needed OR necessar* OR unnecessar* OR declin* OR avoid* OR on-demand) NEAR/5 (resect* OR surg* OR resect* OR esophagectom* OR oesophagectom*)))) AND ((chemoradi* OR radiochemo* OR (chemotherap* NEAR/5 radiotherap*)))) | 248 |
| Scopus | TITLE-ABS-KEY(((((esophag* OR oesophag*) W/5 (cancer* OR neoplas* OR carcino* OR adenocarcino* OR tumor* OR tumour* OR malign*)))) AND ((((watch* OR see) W/2 wait*) OR (active* W/2 surveil*) OR ((selective* OR needed OR necessar* OR unnecessar* OR declin* OR avoid* OR on-demand) W/2 (resect* OR surg* OR resect* OR esophagectom* OR oesophagectom*)))) AND ((chemoradi* OR radiochemo* OR (chemotherap* W/5 radiotherap*)))) | 5 |
| Total | 753 | |
| Database . | Search . | Hits . |
|---|---|---|
| Embase | (‘esophagus cancer’/exp OR ‘esophagus tumor’/de OR (((esophag* OR oesophag*) NEAR/6 (cancer* OR neoplas* OR carcino* OR adenocarcino* OR tumor* OR tumour* OR malign*))): ab, ti) AND (‘watchful waiting’/de OR (((watch* OR see) NEAR/3 wait*) OR (active* NEAR/3 surveil*) OR ((selective* OR reserv* OR selected* OR needed OR necessar* OR unnecessar* OR declin* OR avoid* OR on-demand) NEAR/6 (resect* OR surg* OR resect* OR esophagectom* OR oesophagectom*))): ab, ti) AND (‘chemoradiotherapy’/exp OR (chemoradi* OR radiochemo* OR (chemotherap* NEAR/6 radiotherap*)): ab, ti) | 284 |
| Medline Orvid | (‘Esophageal Neoplasms’/OR (((esophag* OR oesophag*) ADJ6 (cancer* OR neoplas* OR carcino* OR adenocarcino* OR tumor* OR tumour* OR malign*))).ab, ti.) AND (‘Watchful Waiting’/OR (((watch* OR see) ADJ3 wait*) OR (active* ADJ3 surveil*) OR ((selective* OR needed OR necessar* OR unnecessar* OR declin* OR avoid* OR on-demand) ADJ6 (resect* OR surg* OR resect* OR esophagectom* OR oesophagectom*))).ab, ti.) AND (exp ‘Chemoradiotherapy’/OR (‘Chemotherapy, Adjuvant’/AND ‘Radiotherapy, Adjuvant’/) OR (chemoradi* OR radiochemo* OR (chemotherap* ADJ6 radiotherap*)).ab, ti.) | 106 |
| Cochrane | ((((esophag* OR oesophag*) NEAR/6 (cancer* OR neoplas* OR carcino* OR adenocarcino* OR tumor* OR tumour* OR malign*))): ab, ti) AND ((((watch* OR see) NEAR/3 wait*) OR (active* NEAR/3 surveil*) OR ((selective* OR needed OR necessar* OR unnecessar* OR declin* OR avoid* OR on-demand) NEAR/6 (resect* OR surg* OR resect* OR esophagectom* OR oesophagectom*))): ab, ti) AND ((chemoradi* OR radiochemo* OR (chemotherap* NEAR/6 radiotherap*)): ab, ti) | 110 |
| Web of science | TS = (((((esophag* OR oesophag*) NEAR/5 (cancer* OR neoplas* OR carcino* OR adenocarcino* OR tumor* OR tumour* OR malign*)))) AND ((((watch* OR see) NEAR/2 wait*) OR (active* NEAR/2 surveil*) OR ((selective* OR needed OR necessar* OR unnecessar* OR declin* OR avoid* OR on-demand) NEAR/5 (resect* OR surg* OR resect* OR esophagectom* OR oesophagectom*)))) AND ((chemoradi* OR radiochemo* OR (chemotherap* NEAR/5 radiotherap*)))) | 248 |
| Scopus | TITLE-ABS-KEY(((((esophag* OR oesophag*) W/5 (cancer* OR neoplas* OR carcino* OR adenocarcino* OR tumor* OR tumour* OR malign*)))) AND ((((watch* OR see) W/2 wait*) OR (active* W/2 surveil*) OR ((selective* OR needed OR necessar* OR unnecessar* OR declin* OR avoid* OR on-demand) W/2 (resect* OR surg* OR resect* OR esophagectom* OR oesophagectom*)))) AND ((chemoradi* OR radiochemo* OR (chemotherap* W/5 radiotherap*)))) | 5 |
| Total | 753 | |
Inclusion criteria were: patients had esophageal cancer, underwent nCRT (regimen not specified), had a clinically complete response during response evaluation after neoadjuvant treatment (diagnostic modalities not specified) and were subjected to active surveillance after neoadjuvant treatment. Publications other than systematic reviews, randomized controlled trials, cohort studies, case-control studies or patient series were excluded.
Results
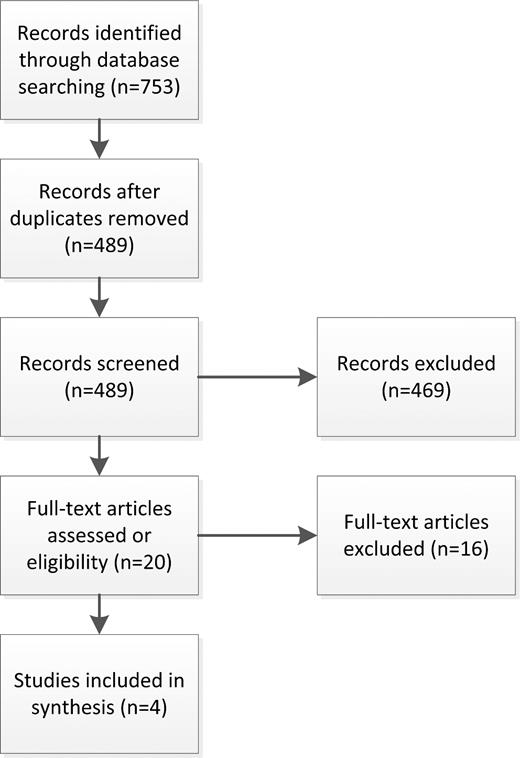
We identified 489 unique records from the database search. A total of 20 articles concerning active surveillance after nCRT for esophageal cancer were identified based on title/abstract screening. Full text screening resulted in the final selection of four articles (Fig. 3).
Flowchart for systematic review on clinical outcomes after active surveillance.
Some 61 patients with squamous cell carcinoma (n = 18), adenocarcinoma (n = 40) or other cancer type (n = 3) from MD Anderson Cancer Center who declined surgery after nCRT had a cCR based on PET-CT and endoscopy with regular biopsies. The 5-year overall survival rate was 58%. Some 12 of 13 patients who developed a locoregional regrowth in the absence of distant metastases during surveillance underwent a radical esophagectomy.27 In line with rectal cancer, these results suggest that a delayed resection can technically be performed in nearly all patients with residual locoregional disease that has been missed initially during response evaluation.30 In a subsequent comparative analysis, 36 patients that underwent active surveillance from the same cohort were matched to 36 patients who underwent nCRT followed by standard surgery using the propensity-score method. Estimated median overall survival was nonsignificantly better in the active surveillance group than in the standard surgery group (58 months, 95% confidence interval [C.I.]: 27.7 to not applicable vs. 51 months, 95% C.I.: 30.7 to not applicable, respectively, p = 0.28). All 11 patients in the active surveillance group with locoregional regrowth in the absence of distant metastases underwent delayed surgery with excellent outcome (median overall survival 58 months). Furthermore, distant dissemination rate (the percentage of patients who developed distant metastases) was comparable in both groups (31% in the active surveillance group and 28% in the standard surgery group).28 These results support the earlier described assumption that dissemination already must have occurred in most patients at time of diagnosis.
A second study from Italy reported on patients that underwent surveillance (n = 38) and patients after planned surgery (n = 39). All patients had a cCR after nCRT for esophageal squamous cell carcinoma. Clinical response was assessed using endoscopy with regular biopsies and patients in the surveillance group were not operated on because they were considered unfit for surgery or declined surgery. Nevertheless, 5-year overall survival rates were comparable in both groups (57% in the active surveillance group vs. 50% in the standard surgery group, p = 0.99).25
Similar outcomes were described by a small Irish study that analyzed 25 patients who underwent nCRT with or without surgery when a cCR was diagnosed after endoscopy post-nCRT.26
Based on the promising results from these explorative (phase I/II) studies, we feel that an active surveillance approach is feasible and can now safely be tested in a phase III trial.
Conclusion and future directions
An active surveillance approach is currently applied only in patients who refuse surgery or are considered unfit for surgery after completion of nCRT. In the near future, an organ preserving strategy may be offered as an alternative treatment to patients with a cCR after completion of nCRT. However, a phase III trial is needed to ascertain that active surveillance does not lead to inferior long-term oncological outcome as compared to standard surgery. At present, two trials, the French ESOSTRATE-trial and the Dutch-SANO trial (Surgery As Needed for esophageal cancer), have been initiated to address this important question.58 Both trials plan to recruit 300 patients each (including adenocarcinoma and squamous cell carcinoma) with a cCR after completion of nCRT. Both trials use different nCRT regimens, with the SANO-trial using the relatively mild CROSS regimen and the ESOSTRATE-trial using higher doses of nCRT. The latter would probably increase pCR rate, but at the cost of an increase in toxicity and postoperative complications, potentially leading to a less beneficial effectivity/toxicity ratio. The primary endpoint of both trials is overall survival. After response evaluation using endoscopy with (bite-on-bite) biopsies, EUS with FNA and 18F-FDG PET-CT, patients with a cCR will be randomized to receive either active surveillance or standard surgery. In both studies, the sample size leads to a noninferiority margin of 15%. Combining outcomes of both trials will reduce this noninferiority margin to 10%, which is in line with other noninferiority oncological clinical trials comparing active surveillance with standard surgery.32 Results of both trials are expected in 2023.
It is anticipated that in the next few years the diagnostic accuracy of tests to assess tumor response to nCRT will improve. Promising results have been published using diffusion-weighted MRI and dynamic contrast-enhanced MRI, but its clinical applicability remains to be proven.59,60 If residual disease and/or local regrowths can be detected more accurately or at an earlier stage than with the current diagnostic modalities, this may reduce the proportion of patients scheduled for a postponed surgical resection and the proportion of patients with irresectable regrowths during active surveillance. Nevertheless, current diagnostic modalities have proven to be sufficiently accurate in response evaluation and detection of local regrowths during active surveillance to justify testing of this promising treatment strategy as potential standard of care.
Acknowledgments
Mr. W.M. Bramer, library Erasmus University Rotterdam, the Netherlands is acknowledged for his assistance in the literature search.
References
Author notes
This paper reflects an invited lecture that was given by J. J. B. van Lanschot during the 15th World Congress of the I.S.D.E. in September 2016, Singapore.