Abstract
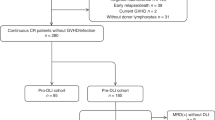
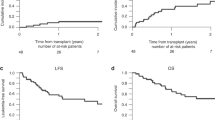
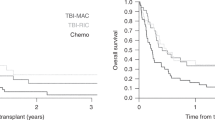
Relapse of pediatric acute lymphoblastic leukemia (ALL) remains the main cause of treatment failure after allogeneic stem cell transplantation (alloSCT). A high level of minimal residual disease (MRD) before alloSCT has been shown to predict these relapses. Patients at risk might benefit from a preemptive alloimmune intervention. In this first prospective, MRD-guided intervention study, 48 patients were stratified according to pre-SCT MRD level. Eighteen children with MRD level ⩾1 × 10−4 were eligible for intervention, consisting of early cyclosporine A tapering followed by consecutive, incremental donor lymphocyte infusions (n=1–4). The intervention was associated with graft versus host disease ⩾grade II in only 23% of patients. Event-free survival in the intervention group was 19%. However, in contrast with the usual early recurrence of leukemia, relapses were delayed up to 3 years after SCT. In addition, several relapses presented at unusual extramedullary sites suggesting that the immune intervention may have altered the pattern of leukemia recurrence. In 8 out of 11 evaluable patients, relapse was preceded by MRD recurrence (median 9 weeks, range 0–30). We conclude that in children with high-risk ALL, immunotherapy-based regimens after SCT are feasible and may need to be further intensified to achieve total eradication of residual leukemic cells.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Pui CH, Evans WE . Acute lymphoblastic leukemia. N Engl J Med 1998; 339: 605–615.
Pui CH, Robison LL, Look AT . Acute lymphoblastic leukaemia. Lancet 2008; 371: 1030–1043.
Balduzzi A, Valsecchi MG, Uderzo C, De LP, Klingebiel T, Peters C et al. Chemotherapy versus allogeneic transplantation for very-high-risk childhood acute lymphoblastic leukaemia in first complete remission: comparison by genetic randomisation in an international prospective study. Lancet 2005; 366: 635–642.
Borgmann A, von Stackelberg A, Hartmann R, Ebell W, Klingebiel T, Peters C et al. Unrelated donor stem cell transplantation compared with chemotherapy for children with acute lymphoblastic leukemia in a second remission: a matched-pair analysis. Blood 2003; 101: 3835–3839.
Bader P, Hancock J, Kreyenberg H, Goulden NJ, Niethammer D, Oakhill A et al. Minimal residual disease (MRD) status prior to allogeneic stem cell transplantation is a powerful predictor for post-transplant outcome in children with ALL. Leukemia 2002; 16: 1668–1672.
Knechtli CJ, Goulden NJ, Hancock JP, Grandage VL, Harris EL, Garland RJ et al. Minimal residual disease status before allogeneic bone marrow transplantation is an important determinant of successful outcome for children and adolescents with acute lymphoblastic leukemia. Blood 1998; 92: 4072–4079.
van der Velden VHJ, Joosten SA, Willemse MJ, van-Wering ER, Lankester A, van Dongen JJM et al. Real-time quantitative PCR for detection of minimal residual disease before allogeneic stem cell transplantation predicts outcome in children with acute lymphoblastic leukemia. Leukemia 2001; 15: 1485–1487.
Krejci O, van der Velden VHJ, Bader P, Kreyenberg H, Goulden N, Hancock J et al. Level of minimal residual disease prior to haematopoietic stem cell transplantation predicts prognosis in paediatric patients with acute lymphoblastic leukaemia: a report of the Pre-BMT MRD Study Group. Bone Marrow Transplant 2003; 32: 849–851.
Sramkova L, Muzikova K, Fronkova E, Krejci O, Sedlacek P, Formankova R et al. Detectable minimal residual disease before allogeneic hematopoietic stem cell transplantation predicts extremely poor prognosis in children with acute lymphoblastic leukemia. Pediatr Blood Cancer 2007; 48: 93–100.
Weisdorf DJ, Nesbit ME, Ramsay NK, Woods WG, Goldman AI, Kim TH et al. Allogeneic bone marrow transplantation for acute lymphoblastic leukemia in remission: prolonged survival associated with acute graft-versus-host disease. J Clin Oncol 1987; 5: 1348–1355.
Atra A, Miller B, Shepherd V, Shankar A, Wilson K, Treleavan J et al. Donor lymphocyte infusion for childhood acute lymphoblastic leukemia relapsing after bone marrow transplantation. Br J Haemat 1997; 97: 165–168.
Passweg JR, Tiberghien P, Cahn JY, Vowels MR, Camitta BM, Gale RP et al. Graft-versus-leukemia effects in T lineage and B lineage acute lymphoblastic leukemia. Bone Marrow Transplant 1998; 21: 153–158.
Sullivan KM, Weiden PL, Storb R, Witherspoon RP, Fefer A, Fisher L et al. Influence of acute and chronic graft-versus-host disease on relapse and survival after bone marrow transplantation from HLA-identical siblings as treatment of acute and chronic leukemia. Blood 1989; 73: 1720–1728.
Horowitz MM, Gale RP, Sondel PM, Goldman JM, Kersey J, Kolb HJ et al. Graft-versus-leukemia reactions after bone marrow transplantation. Blood 1990; 75: 555–562.
Locatelli F, Zecca M, Rondelli R, Bonetti F, Dini G, Prete A et al. Graft versus host disease prophylaxis with low-dose cyclosporine-A reduces the risk of relapse in children with acute leukemia given HLA-identical sibling bone marrow transplantation: results of a randomized trial. Blood 2000; 95: 1572–1579.
Bader P, Kreyenberg H, Hoelle W, Dueckers G, Handgretinger R, Lang P et al. Increasing mixed chimerism is an important prognostic factor for unfavorable outcome in children with acute lymphoblastic leukemia after allogeneic stem-cell transplantation: possible role for pre-emptive immunotherapy? J Clin Oncol 2004; 22: 1696–1705.
Kolb H-J, Schattenberg A, Goldman JM, Hertenstein B, Jacobson N, Arcese W et al. Graft-versus-leukemia effect of donor lymphocyte transfusions in marrow grafted patients. Blood 1995; 86: 2041–2050.
Veerman AJ, Kamps WA, van den BH, van den BE, Bokkerink JP, Bruin MC et al. Dexamethasone-based therapy for childhood acute lymphoblastic leukaemia: results of the prospective Dutch Childhood Oncology Group (DCOG) protocol ALL-9 (1997–2004). Lancet Oncol 2009; 10: 957–966.
Peters C, Schrauder A, Schrappe M, von SA, Stary J, Yaniv I et al. Allogeneic haematopoietic stem cell transplantation in children with acute lymphoblastic leukaemia: the BFM/IBFM/EBMT concepts. Bone Marrow Transplant 2005; 35 (Suppl 1): S9–S11.
Vossen JM, Heidt PJ, van den Berg H, Gerritsen EJA, Hermans J, Dooren LJ . Prevention of infection and graft-versus-host disease by suppression of intestinal microflora in children treated with allogeneic bone marrow transplantation. Eur J Clin Microbiol Infect Dis 1990; 9: 14–22.
Slaper-Cortenbach IC, Wijngaarden-du Bois MJ, Vries-van Rossen A, Borst HP, van der LH, van Heugten HG et al. The depletion of T cells from haematopoietic stem cell transplants. Rheumatology (Oxford) 1999; 38: 751–754.
Glucksberg H, Storb R, Fefer A, Buckner CD, Neiman PE, Clift RA et al. Clinical manifestations of graft-versus-host disease in human recipients of marrow from HLA-matched sibling donors. Transplantation 1974; 18: 295–304.
Verhagen OJ, Willemse MJ, Breunis WB, Wijkhuijs AJ, Jacobs DC, Joosten SA et al. Application of germline IGH probes in real-time quantitative PCR for the detection of minimal residual disease in acute lymphoblastic leukemia. Leukemia 2000; 14: 1426–1435.
van der Velden VHJ, Wijkhuijs JM, Jacobs DC, van Wering ER, van Dongen JJ . T cell receptor gamma gene rearrangements as targets for detection of minimal residual disease in acute lymphoblastic leukemia by real-time quantitative PCR analysis. Leukemia 2002; 16: 1372–1380.
van der Velden VH, Willemse MJ, van der Schoot CE, Hahlen K, van Wering ER, van Dongen JJ . Immunoglobulin kappa deleting element rearrangements in precursor-B acute lymphoblastic leukemia are stable targets for detection of minimal residual disease by real-time quantitative PCR. Leukemia 2002; 16: 928–936.
van Dongen JJ, Langerak AW, Bruggemann M, Evans PA, Hummel M, Lavender FL et al. Design and standardization of PCR primers and protocols for detection of clonal immunoglobulin and T-cell receptor gene recombinations in suspect lymphoproliferations: report of the BIOMED-2 Concerted Action BMH4-CT98-3936. Leukemia 2003; 17: 2257–2317.
Bruggemann M, van der Velden VHJ, Raff T, Droese J, Ritgen M, Pott C et al. Rearranged T-cell receptor beta genes represent powerful targets for quantification of minimal residual disease in childhood and adult T-cell acute lymphoblastic leukemia. Leukemia 2004; 18: 709–719.
van der Velden VH, de BM, van Wering ER, van Dongen JJ . Immunoglobulin light chain gene rearrangements in precursor-B-acute lymphoblastic leukemia: characteristics and applicability for the detection of minimal residual disease. Haematologica 2006; 91: 679–682.
van der Velden VH, Cazzaniga G, Schrauder A, Hancock J, Bader P, Panzer-Grumayer ER et al. Analysis of minimal residual disease by Ig/TCR gene rearrangements: guidelines for interpretation of real-time quantitative PCR data. Leukemia 2007; 21: 604–611.
van Dongen JJ, Seriu T, Panzer-Grumayer ER, Biondi A, Pongers-Willemse MJ, Corral L et al. Prognostic value of minimal residual disease in acute lymphoblastic leukaemia in childhood. Lancet 1998; 352: 1731–1738.
Flohr T, Schrauder A, Cazzaniga G, Panzer-Grumayer R, Van der Velden V, Fischer S et al. Minimal residual disease-directed risk stratification using real-time quantitative PCR analysis of immunoglobulin and T-cell receptor gene rearrangements in the international multicenter trial AIEOP-BFM ALL 2000 for childhood acute lymphoblastic leukemia. Leukemia 2008; 22: 771–782.
van der Velden V, Hoogeveen PG, Pieters R, van Dongen JJ . Impact of two independent bone marrow samples on minimal residual disease monitoring in childhood acute lymphoblastic leukaemia. Br J Haematol 2006; 133: 382–388.
Putter H, Fiocco M, Geskus RB . Tutorial in biostatistics: competing risks and multi-state models. Stat Med 2007; 26: 2389–2430.
Bader P, Kreyenberg H, Henze GH, Eckert C, Reising M, Willasch A et al. Prognostic value of minimal residual disease quantification before allogeneic stem-cell transplantation in relapsed childhood acute lymphoblastic leukemia: the ALL-REZ BFM Study Group. J Clin Oncol 2009; 27: 377–384.
Takami A, Okumura H, Yamazaki H, Kami M, Kim SW, Asakura H et al. Prospective trial of high-dose chemotherapy followed by infusions of peripheral blood stem cells and dose-escalated donor lymphocytes for relapsed leukemia after allogeneic stem cell transplantation. Int J Hematol 2005; 82: 449–455.
Huck K, Laws HJ, Meisel R, Traeger A, Bernbeck B, Schonberger S et al. Three cases of renal relapse after allogeneic hematopoietic stem cell transplantation for childhood acute lymphoblastic leukemia. Haematologica 2006; 91 (5 Suppl): ECR07.
Choi SJ, Lee JH, Lee JH, Kim S, Seol M, Lee YS et al. Treatment of relapsed acute myeloid leukemia after allogeneic bone marrow transplantation with chemotherapy followed by G-CSF-primed donor leukocyte infusion: a high incidence of isolated extramedullary relapse. Leukemia 2004; 18: 1789–1797.
Chong G, Byrnes G, Szer J, Grigg A . Extramedullary relapse after allogeneic bone marrow transplantation for haematological malignancy. Bone Marrow Transplant 2000; 26: 1011–1015.
Zeiser R, Bertz H, Spyridonidis A, Houet L, Finke J . Donor lymphocyte infusions for multiple myeloma: clinical results and novel perspectives. Bone Marrow Transplant 2004; 34: 923–928.
Vago L, Perna SK, Zanussi M, Mazzi B, Barlassina C, Stanghellini MT et al. Loss of mismatched HLA in leukemia after stem-cell transplantation. N Engl J Med 2009; 361: 478–488.
Collins RHJ, Shpilberg O, Drobyski WR, Porter DL, Giralt S, Champlin R et al. Donor leukocyte infusions in 140 patients with relapsed malignancy after allogeneic bone marrow transplantation [see comments]. J Clin Oncol 1997; 15: 433–444.
Kolb HJ, Mittermuller J, Clemm C, Holler E, Ledderose G, Brehm G et al. Donor leukocyte transfusions for treatment of recurrent chronic myelogenous leukemia in marrow transplant patients. Blood 1990; 76: 2462–2465.
Riddell SR, Murata M, Bryant S, Warren EH . T-cell therapy of leukemia. Cancer Control 2002; 9: 114–122.
Klingebiel T, Bader P . Delayed lymphocyte infusion in children given SCT. Bone Marrow Transplant 2008; 41 (Suppl 2): S23–S26.
Kolb HJ, Schmid C, Barrett AJ, Schendel DJ . Graft-versus-leukemia reactions in allogeneic chimeras. Blood 2004; 103: 767–776.
van der Harst D, Goulmy E, Falkenburg JH, Kooij-Winkelaar YM, Luxemburg-Heijs SA, Goselink HM et al. Recognition of minor histocompatibility antigens on lymphocytic and myeloid leukemic cells by cytotoxic T-cell clones. Blood 1994; 83: 1060–1066.
Cardoso AA, Seamon MJ, Afonso HM, Ghia P, Boussiotis VA, Freeman GJ et al. Ex vivo generation of human anti-pre-B leukemia-specific autologous cytolytic T cells. Blood 1997; 90: 549–561.
D’Amico G, Bonamino M, Dander E, Marin V, Basso G, Balduzzi A et al. T cells stimulated by CD40L positive leukemic blasts-pulsed dendritic cells meet optimal functional requirements for adoptive T-cell therapy. Leukemia 2006; 20: 2015–2024.
Jedema I, Meij P, Steeneveld E, Hoogendoorn M, Nijmeijer BA, van de MM et al. Early detection and rapid isolation of leukemia-reactive donor T cells for adoptive transfer using the IFN-gamma secretion assay. Clin Cancer Res 2007; 13 (2 Part 1): 636–643.
Hartwig M, Weigel S, Bernig T, Bader P, Dolken R, Beck J . Maintenance immunotherapy by repetitive low-dose donor lymphocytes infusions in a child with relapse state AML after allogeneic stem cell transplantation. Pediatr Hematol Oncol 2007; 24: 137–140.
Bader P, Koscielniak E, Schlegel PG, Kors A, Lankester A, Kreyenberg H et al. Combined chemo-immunotherapy in children with ALL who relapse after allogeneic stem cell transplantation—an option to induce long term remission. Bone Marrow Transplant 2004; 33: s220.
Berthou C, Leglise MC, Herry A, Balcon D, Hardy E, Lessard M et al. Extramedullary relapse after favorable molecular response to donor leukocyte infusions for recurring acute leukemia. Leukemia 1998; 12: 1676–1681.
Acknowledgements
We thank Professor Dr M Tilanus for the analysis of chimerism, Dr CE van der Schoot and C Homburg for MRD analysis of selected samples and Monique ten Dam, Remy van der Hulst, Ada Struyk, Els Jol-van der Zijde, Maaike de Bie and Patricia Hoogeveen for technical assistance. We also acknowledge the support of the staff of the DCOG laboratory in The Hague, The Netherlands, for sample handling and analysis. This research was supported by Grant UL 2001-2515 from the Dutch Cancer Society (KWF, Amsterdam).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Lankester, A., Bierings, M., van Wering, E. et al. Preemptive alloimmune intervention in high-risk pediatric acute lymphoblastic leukemia patients guided by minimal residual disease level before stem cell transplantation. Leukemia 24, 1462–1469 (2010). https://doi.org/10.1038/leu.2010.133
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2010.133
Keywords
This article is cited by
-
Influence of pre-transplant minimal residual disease on prognosis after Allo-SCT for patients with acute lymphoblastic leukemia: systematic review and meta-analysis
BMC Cancer (2018)
-
Minimal residual disease assessment by next-generation sequencing. Better tools to gaze into the crystal ball?
Bone Marrow Transplantation (2017)
-
Next-generation sequencing indicates false-positive MRD results and better predicts prognosis after SCT in patients with childhood ALL
Bone Marrow Transplantation (2017)
-
Comparison of outcomes after donor lymphocyte infusion with or without prior chemotherapy for minimal residual disease in acute leukemia/myelodysplastic syndrome after allogeneic hematopoietic stem cell transplantation
Annals of Hematology (2017)
-
Reduction of Minimal Residual Disease in Pediatric B-lineage Acute Lymphoblastic Leukemia by an Fc-optimized CD19 Antibody
Molecular Therapy (2016)