Abstract
The effectiveness of surgery in patients with sciatica due to lumbar disc herniations is not without dispute. The goal of this study was to assess the effects of surgery versus conservative therapy (including epidural injections) for patients with sciatica due to lumbar disc herniation. A comprehensive search was conducted in MEDLINE, EMBASE, CINAHL, CENTRAL, and PEDro up to October 2009. Randomised controlled trials of adults with lumbar radicular pain, which evaluated at least one clinically relevant outcome measure (pain, functional status, perceived recovery, lost days of work) were included. Two authors assessed risk of bias according to Cochrane criteria and extracted the data. In total, five studies were identified, two of which with a low risk of bias. One study compared early surgery with prolonged conservative care followed by surgery if needed; three studies compared surgery with usual conservative care, and one study compared surgery with epidural injections. Data were not pooled because of clinical heterogeneity and poor reporting of data. One large low-risk-of-bias trial demonstrated that early surgery in patients with 6–12 weeks of radicular pain leads to faster pain relief when compared with prolonged conservative treatment, but there were no differences after 1 and 2 years. Another large low-risk-of-bias trial between surgery and usual conservative care found no statistically significant differences on any of the primary outcome measures after 1 and 2 years. Future studies should evaluate who benefits more from surgery and who from conservative care.
Similar content being viewed by others
Introduction
The prevalence of sciatic symptoms reported in the literature varies considerably ranging from 1.6% in the general population to 43% in a selected working population [8]. Although the prognosis is good in most patients [9], a substantial proportion (up to 30%) continues to have pain for 1 year or longer [18, 20]. In approximately 90% of the cases, sciatica is caused by a herniated disc involving nerve root compression. However, lumbar canal stenosis or foraminal stenosis and (less often) tumours or cysts are other possible causes [15].
The most important symptom of sciatica is lumbosacral radicular leg pain that follows a dermatomal pattern radiating below the knee and into the foot and toes [15, 17]. The pain worsens with coughing; patients may report sensory symptoms, limited forward flexion of the lumbar spine, gait deformity and unilateral spasm of the paraspinal muscles. However, most patients present with a less clear clinical picture. In acute sciatica, diagnostic imaging may only be indicated if there are indications of underlying pathology (e.g. infections, malignancies) other than disc herniation. In patients with persistent and severe symptoms who fail to improve following 6–8 weeks of non-surgical treatment, imaging might be useful to identify the presence or absence of a herniated disc with nerve root compression [15].
Management of sciatica varies considerably. Patients are commonly treated in primary care but a small proportion is referred to secondary care and may eventually undergo surgery if complaints remain present for at least 6 weeks. Conservative treatment for sciatica is primarily aimed at pain reduction, either by analgesics or by reducing pressure on the nerve root. There seems to be consensus that surgery is indicated in carefully selected patients for sciatica in presence of a herniated lumbar disc [6], or severe sciatica with serious or progressive neurologic deficits and imaging demonstrating lumbar disc herniation at the nerve root level correlating with the patient’s examination findings [7, 9]. The primary rationale of surgery for sciatica is that surgery will relieve nerve root irritation or compression due to herniated disc material. The most common type of surgery is open microdiscectomy, surgical removal of part of the disc, performed with or without the use of an operating microscope or other magnifying tools. Other minimally invasive surgical techniques, such as endoscopic surgery have recently been developed [4]. In the absence of serious neurologic deficits or for persistent non-radicular low back pain, consensus whether surgery is useful or not has not yet been established. Furthermore, the timing of the intervention with respect to prolonged conservative care has not been evaluated properly.
At present, several randomised trials have been published that have compared surgery with conservative treatment. The objective of this systematic review is to compare and summarise the evidence regarding the effectiveness of surgery compared with conservative treatment for patients with sciatica due to lumbar disc herniation.
Methods
Search methods for identification of studies
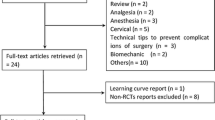
A comprehensive search was conducted by an experienced librarian in several databases of medical literature: MEDLINE, EMBASE, CINAHL, CENTRAL (the Cochrane Central Register of Controlled Trials), PEDro, and ICL up to October 2009. The search strategy is given in Table 1. References from the included studies were also screened and experts approached in order to identify additional primary studies not previously identified. Two review authors (MA, WP) working independently from one another examined titles and abstracts from the electronic search. Full articles were obtained if necessary. A third reviewer was consulted (MvT), if consensus was not reached.
Criteria for considering studies for this review
References were selected if they met all of the following selection criteria:
-
The study was stated to be a randomised controlled trial.
-
The study compared surgery to non-surgical interventions (i.e. epidural injections, conservative therapy).
-
The patients included were adult (>18 years of age) subjects with sciatica due to a herniated disc.
-
The outcome(s) evaluated included at least one of the main clinically relevant outcome measures (i.e. pain, functional status, recovery, or sick leave) using a valid instrument.
-
The follow-up was at least 1 day.
-
The language was limited to English, Dutch and German.
The following self-reported measures were assessed and considered as the primary outcomes: leg pain and/or back pain, leg pain specific functional status, perceived recovery (e.g. subjective overall improvement, proportion of patients recovered), and lost days at work (e.g. return to work status, number of days off work or with sick leave). Any other outcome was considered as secondary (e.g. SF-36 reporting on bodily pain). Physiological variables, such as spinal flexibility and number of degrees of straight-leg raising were not assessed since it is believed that these outcomes correlate poorly with clinical status.
Assessment of risk of bias for the included studies
Two review authors (SR and MM) working independently of each other conducted the risk-of-bias assessment and data extraction. Risk of bias of the individual studies was assessed using the criteria list advised by the Cochrane Back Review Group (CBRG) [5], which consists of 11 items that assess internal validity. Items and operationalisation are given in Table 2. Items were scored as positive if they fulfilled the criteria, negative when bias was likely or marked as inconclusive if there was insufficient information. Differences in the scoring of the risk-of-bias assessment and data extraction were discussed during a consensus meeting. The item for compliance was not scored because this item was irrelevant for single-session interventions, such as surgery. A study with a low risk of bias was defined as fulfilling six or more of the validity items.
Data collection and analysis
Included studies were categorised under separate comparisons with clinically homogeneous characteristics. An a priori list of items was used for the data extraction, consisting of both descriptive data (e.g. study population, type of interventions) and quantitative data regarding the primary and secondary outcome measures. With sufficient clinically and statistically homogeneous and comparable reported outcomes, data was planned to be pooled with the aid of Revman 5. To identify publication bias, funnel plots were planned to be examined. In case meta-analysis was not feasible, a best evidence synthesis was anticipated using low-risk-of-bias studies. The overall quality of the evidence was graded as “High”, “Moderate”, “Low”, or “Very low”, according to the GRADE approach by Furlan et al. [5]. Single studies were considered imprecise (i.e. sparse data) and provide “low quality evidence”, which could be further downgraded to “very low quality evidence” if there were also limitations in design or indirectness.
Results
Search and selection results
The search yielded 2,383 citations. In total, five studies were identified [2, 12, 13, 19, 22]. Three comparisons were evaluated: (1) one study compared early surgery with prolonged conservative care for 6 months followed by surgery if needed [13], (2) three studies contrasted surgery with “usual conservative care” [12, 19, 22], and (3) one study contrasted surgery with epidural injections [2].
Risk-of-bias assessment
The results for the risk-of-bias assessment are given in Table 3. Of the five identified studies, two were thought to have a low risk of bias, both of which also applied adequate allocation concealment [13, 22]. Although compliance was not formally evaluated because surgery is considered a single-session intervention, this nevertheless is an important item. In the study by Weinstein et al. [22], for example, adherence to the assigned treatment group was severely limited, i.e. 50% of the patients assigned to surgery actually received surgery within 3 months of enrolment, while 30% of those patients assigned to non-operative treatment received surgery in the same period. In the study by Butterman et al. [2], more than half of those patients assigned to epidural injections considered the treatment a failure and underwent subsequent discectomy, which on average was 4.5 months following the onset of symptoms. In another study, a substantial proportion of patients assigned to conservative care received surgery at follow-up [13]; however, that study was designed to evaluate the timing of surgery and part of the control group randomised to prolonged conservative care was expected to receive surgery during follow-up.
Effects of the interventions
Due to poor reporting of data in the studies of Weber et al. [19] and Osterman et al. [12], these studies comparing surgery with usual conservative care could not be pooled. The comparisons ‘surgery versus epidural injections’ and ‘early surgery versus prolonged conservative care’ were each investigated in only one trial. The characteristics of the included trials are given in Table 4. The results of the five included trials are given in Table 5. The few number of studies identified per outcome made a funnel plot unfeasible.
Early surgery versus prolonged conservative care
One large randomised trial (n = 283) with a low risk of bias compared early surgery to prolonged conservative treatment followed by surgery if needed in patients with severe sciatica for 6–12 weeks [13]. Of the patients, 89% randomised to early surgery underwent microdiscectomy after a mean of 2 weeks, while 39% of patients randomised to conservative treatment underwent surgery after a mean of 19 weeks. Relief of leg pain was faster for patients assigned to early surgery. Intention-to-treat analysis showed statistically significant more leg pain relief in favour of early surgery as compared with prolonged conservative care at 3 months (MD −17.70, 95% CI −23.1 to −12.3). There was no significant overall difference between the two groups in disability scores during the first year. The median time to recovery was 4.0 weeks [95% confidence interval (CI), 3.7–4.4] for early surgery and 12.1 weeks (95% CI, 9.5–14.9) for prolonged conservative treatment. During the first year, early surgery achieved a faster rate of perceived recovery with a hazard ratio of 1.97 (95% CI 1.72–2.22, P < 0.001). At 1 year of follow-up, however, 95% of patients in both treatment groups had experienced satisfactory recovery, and no subsequent differences were found. This lack of a difference between groups was maintained for the following year. In conclusion, one low-risk-of-bias study yielded a low level of evidence (GRADE) to the effect that early surgery was beneficial for pain relief as compared to prolonged conservative care in the short term, but not in the longer term with a faster recovery rate for early surgery.
Surgery versus usual conservative care
One old study (n = 126) with a high risk of bias compared long-term outcomes of discectomy to conservative management [19]. Both patient and observer ratings demonstrated that discectomy was significantly better than conservative treatment at 1 year. After 1 year, 24 of the 66 patients (36%) in the conservative care group versus 39 of the 60 patients (65%) in the surgery group reported a good outcome. No significant differences in outcomes were reported at 4 and 10 years follow-up.
One small trial (n = 56) with a high risk of bias compared microdiscectomy with conservative treatment in patients with sciatica for 6–12 weeks [12]. Overall, no significant differences were found for leg pain or back pain, and subjective disability throughout the 2 years of follow-up. VAS leg pain scores, however, improved more rapidly in the discectomy group; 6 weeks scores in the surgery group was 12 (SD 20) versus 25 (SD 27) in the conservative group. The per-protocol analysis demonstrated no statistically significant differences.
A large trial (n = 501) with a low risk of bias in patients with sciatica for at least 6 weeks and confirmed disc herniation showed that both the surgery as well as the conservative treatment group improved substantially over 2 years for all primary and secondary outcome measures [22]. The intention-to-treat analysis showed no statistically significant differences for any of the primary outcome measures. Of the patients randomised to surgery, 50% received surgery within 3 months of inclusion as compared with 30% who received surgery in the group randomised to conservative treatment. After 2 years of follow-up, 45% of patients in the conservative treatment group underwent surgery and 40% in the surgery group received conservative treatment.
In conclusion, there is conflicting evidence as to whether surgery is more beneficial than conservative care for short- and long-term follow-up.
Surgery versus epidural steroid injections
One trial (n = 100) with a high risk of bias was identified that compared results following microdiscectomy with results after epidural steroid injection [2]. Patients undergoing discectomy had the most rapid decrease in their symptoms. The decrease in leg pain in the discectomy group was significantly greater than in the epidural steroid injection group at 3- and 6-month follow-up intervals, but not beyond 1 year. There were no significant differences between groups for back pain throughout the follow-up. Of the 50 patients, 27 who received a steroid injection had a subsequent microdiscectomy. Outcomes in this cross-over group were similar to those of the surgery group. In conclusion, there is very low quality evidence (high risk of bias) that discectomy was beneficial over epidural steroid injections for the short term only.
Discussion
In this review we identified five studies comparing surgery with conservative care. Only one low-risk-of-bias study compared early surgery to prolonged conservative care [13] and demonstrated more relief of leg pain up to 3 months for early surgery, but at 1 year the differences disappeared. The trials of surgery versus usual conservative treatment showed inconsistent findings. One low-risk-of-bias study compared surgery versus conservative treatment [22] and found no differences between the two treatments. We were unable to perform a meta-analysis of these three studies because of the poor data presented in two of the studies. An observational cohort study conducted alongside one trial included 743 patients that received their preferred treatment. Both groups improved substantially over time, but surgery showed significantly better results for pain and function as compared with conservative treatment [21].
Three of the five studies found an effect in the early postoperative period, which diminished during further follow-up. This is relevant because a faster recovery rate could, besides the clinical benefit, have an economic advantage in a relatively young patient population. A cost-effectiveness study performed alongside the trial of Peul et al. [13] showed that surgery is cost-effective with a willingness to pay 40,000 € as per quality-adjusted life years (QALY) [16]. In relation to this, timing of treatment is under debate, but for a reliable analysis of the effect of different timing, information about duration of symptoms is needed. The duration between onset of symptoms and actual treatment is described in four of the five trials [2, 12, 13, 19]. Equally important is the timing of the treatment after diagnosis by protocol or waiting list. This is only reported in two of the trials being 2 weeks [2, 13]. Heterogeneity in the duration of the symptoms or in the timing of treatments introduces a difference in timing of treatment since the onset of complaints and thus bias in the analysis of recovery rate.
The duration and intensity of the conservative treatment is poorly described in the included studies. There are many treatment regimens and modalities available for conservative treatment of sciatica [18] varying from steroids [14] to traction [3] to physiotherapy interventions [10]. Evidence from systematic reviews of conservative interventions for sciatica fail to identify the effect of one intervention over the other, however, large studies with a low risk of bias are scarce [11]. In order to make an informed decision about the clinical homogeneity of the included comparisons, detailed information about the treatments is essential and the denomination “conservative treatment” is not sufficient.
Three narrative reviews which examined choice of surgery or conservative care concluded that surgery is indicated in presence of persistent neuromotor deficit [1, 7, 9]. Both Awad and Moskovich [1] and Legrand et al. [9] suggested to let the patient make an informed choice. The review of Awad and Moskovich [1] was published before publication of three of the studies included in this review [12, 13, 22]. Although the publication of Legrand et al. was in 2007, this study did not include two studies [2, 12] published before that date. Gregory et al. [7] promoted surgery with persistent neuromotor deficit or severe sciatica with a positive straight-leg-raise test and imaging demonstrating lumbar disc herniation at the nerve root level correlating with the patient’s examination findings. Although published in October 2008, this study did not include three studies [2, 12, 19] published before that date. Both reviews did not describe their search strategy, selection methods or quality assessments of the included studies and are therefore, potentially, prone to bias.
Strengths and limitations
There are some limitations in our present review. Firstly, the limited amount of studies, especially those with a low risk of bias, limits the strength of our recommendations. The GRADE approach needs consistent findings in separate studies to raise the level of evidence to ‘moderate’ or ‘high’. The overall quality of the evidence should not be misinterpreted as the quality of an individual study.
A more general problem lies within the methodology of research for the assessment of timing of interventions. Current research models, with the randomised clinical trial as the gold standard, do not allow for a proper analysis of the difference between the time from inclusion (or onset of symptoms) to intervention and prolonged control intervention. The design and analysis of studies is complicated by the difference in cross-over possibilities between the two interventions. Crossing over from conservative treatment to surgery is to be expected for a certain amount of patients. The reverse is also possible as shown in the study of Weinstein et al. [22]. The mechanism is however different as crossing over is only counted as surgery did not take place at all.
The clinical data seem to favour surgery slightly; however, the costs of surgery are likely to be higher than conservative treatment for patients or the health care system. Also, potential complications are probably more prevalent and more severe with surgery. Only from a societal perspective it might be more cost-effective because of lower cost of production loss [16]. Evaluating conservative treatment and surgical intervention requires a different set of outcome parameters, including complications, re-surgeries and economical information to allow for a balanced and informed cost-complication-effectiveness decision.
Conclusions
In general, there is evidence that early surgery in patients with sciatica provides for a better short-term relief of leg pain as compared to prolonged conservative care, but the evidence is low quality because of the fact that only one trial investigated this properly. No significant differences were found between surgery and usual conservative care in any of the clinical outcomes after 1 and 2 years, but the evidence is of very low quality. The scarcity of studies as well as the limited quality of the studies does not support the choice for any timing in our current guidelines.
Future studies should evaluate who benefits more from surgery and who from conservative care. Also economic evaluations should analyse the economical gain of the potential faster recovery against increased cost and complication rate of surgery.
References
Awad JN, Moskovich R (2006) Lumbar disc herniations: surgical versus nonsurgical treatment. Clin Orthop Relat Res 443:183–197
Buttermann GR (2004) Treatment of lumbar disc herniation: epidural steroid injection compared with discectomy. A prospective, randomized study. J Bone Joint Surg Am 86-A:670–679
Clarke J, van TM, Blomberg S, de VH, van der Heijden G, Bronfort G (2006) Traction for low back pain with or without sciatica: an updated systematic review within the framework of the Cochrane collaboration. Spine (Phila Pa 1976) 31:1591–1599
Foley K, Smith MM (1997) Microendoscopic discectomy. Tech Neurosurg 3:301–307
Furlan A, Pennick V, Bombardier C, van Tulder M (2009) 2009 Updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine 34:1929–1941
Gibson JNA, Waddell G (2007) Surgical interventions for lumbar disc prolapse. Cochrane Database of Systematic Reviews CD001350. doi:10.1002/14651858.CD001350.pub4
Gregory DS, Seto CK, Wortley GC, Shugart CM (2008) Acute lumbar disk pain: navigating evaluation and treatment choices. Am Fam Physician 78:835–842
Konstantinou K, Dunn KM (2008) Sciatica: review of epidemiological studies and prevalence estimates. Spine (Phila Pa 1976) 33:2464–2472
Legrand E, Bouvard B, Audran M, Fournier D, Valat JP (2007) Sciatica from disk herniation: medical treatment or surgery? Joint Bone Spine 74:530–535
Luijsterburg PA, Verhagen AP, Ostelo RW, van den Hoogen HJ, Peul WC, Avezaat CJ, Koes BW (2008) Physical therapy plus general practitioners’ care versus general practitioners’ care alone for sciatica: a randomised clinical trial with a 12-month follow-up. Eur Spine J 17:509–517
Luijsterburg PA, Verhagen AP, Ostelo RW, van Os TA, Peul WC, Koes BW (2007) Effectiveness of conservative treatments for the lumbosacral radicular syndrome: a systematic review. Eur Spine J 16:881–899
Osterman H, Seitsalo S, Karppinen J, Malmivaara A (2006) Effectiveness of microdiscectomy for lumbar disc herniation: a randomized controlled trial with 2 years of follow-up. Spine (Phila Pa 1976) 31:2409–2414
Peul WC, van Houwelingen HC, van den Hout WB, Brand R, Eekhof JA, Tans JT, Thomeer RT, Koes BW (2007) Surgery versus prolonged conservative treatment for sciatica. N Engl J Med 356:2245–2256
Price C, Arden N, Coglan L, Rogers P (2005) Cost-effectiveness and safety of epidural steroids in the management of sciatica. Health Technol Assess 9:1–58, iii
Valat JP, Genevay S, Marty M, Rozenberg S, Koes B (2010) Sciatica. Best Pract Res Clin Rheumatol 24:241–252
van den Hout WB, Peul WC, Koes BW, Brand R, Kievit J, Thomeer RT (2008) Prolonged conservative care versus early surgery in patients with sciatica from lumbar disc herniation: cost utility analysis alongside a randomised controlled trial. BMJ 336:1351–1354
van Tulder M, Peul W, Koes B (2010) Sciatica: what the rheumatologist needs to know. Nat Rev Rheumatol 6:139–145
Vroomen PC, de Krom MC, Slofstra PD, Knottnerus JA (2000) Conservative treatment of sciatica: a systematic review. J Spinal Disord 13:463–469
Weber H (1983) Lumbar disc herniation. A controlled, prospective study with ten years of observation. Spine (Phila Pa 1976) 8:131–140
Weber H, Holme I, Amlie E (1993) The natural course of acute sciatica with nerve root symptoms in a double-blind placebo-controlled trial evaluating the effect of piroxicam. Spine (Phila Pa 1976) 18:1433–1438
Weinstein JN, Lurie JD, Tosteson TD, Skinner JS, Hanscom B, Tosteson AN, Herkowitz H, Fischgrund J, Cammisa FP, Albert T, Deyo RA (2006) Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT) observational cohort. JAMA 296:2451–2459
Weinstein JN, Tosteson TD, Lurie JD, Tosteson AN, Hanscom B, Skinner JS, Abdu WA, Hilibrand AS, Boden SD, Deyo RA (2006) Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT): a randomized trial. JAMA 296:2441–2450
Acknowledgments
This study was supported by a grant from the Dutch Health Insurance Council.
Conflict of interest
None.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Jacobs, W.C.H., van Tulder, M., Arts, M. et al. Surgery versus conservative management of sciatica due to a lumbar herniated disc: a systematic review. Eur Spine J 20, 513–522 (2011). https://doi.org/10.1007/s00586-010-1603-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-010-1603-7