Abstract
Purpose
Our goal was to validate the hypothesis that the lumbosacral angle (LSA) increases in children with spinal dysraphism who present with progressive symptoms and signs of tethered cord syndrome (TCS), and if so, to determine for which different types and/or levels the LSA would be a valid indicator of progressive TCS. Moreover, we studied the influence of surgical untethering and eventual retethering on the LSA.
Methods
We retrospectively analyzed the data of 33 children with spinal dysraphism and 33 controls with medulloblastoma. We measured the LSA at different moments during follow-up and correlated this with progression in symptomatology.
Results
LSA measurements had an acceptable intra- and interobserver variability, however, some children with severe deformity of the caudal part of the spinal column, and for obvious reasons those with caudal regression syndrome were excluded. LSA measurements in children with spinal dysraphism were significantly different from the control group (mean LSA change, 21.0° and 3.1° respectively). However, both groups were not age-matched, and when dividing both groups into comparable age categories, we no longer observed a significant difference. Moreover, we did not observe a significant difference between 26 children with progressive TCS as opposed to seven children with stable TCS (mean LSA change, 20.6° and 22.4° respectively).
Conclusions
We did not observe significant differences in LSA measurements for children with clinically progressive TCS as opposed to clinically stable TCS. Therefore, the LSA does not help the clinician to determine if there is significant spinal cord tethering, nor if surgical untethering is needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spinal dysraphism is often associated with tethered cord syndrome (TCS). TCS is a diverse clinical entity supposedly due to abnormal tension on the spinal cord [1–3], in which typical neuroimaging features, such as caudal and/or dorsal displacement of the conus with enlargement of the ventral subarachnoid space, support the diagnosis [3, 4]. Tethering usually occurs at the more caudal segments of the cord in association with a low lying conus [1]. However, tethering of the cervical or thoracic cord, as well as tethering of the caudal segments of the cord despite a normally positioned conus may also be encountered [2]. The latter condition is often termed ‘occult tethered cord syndrome’ [5]. The clinical presentation of TCS is quite divers, including neurologic, urologic, orthopaedic and/or gastrointestinal symptoms and signs. Clinical deterioration in one or more of these categories may be subtle or slowly progressive and therefore difficult to interpret, or even inconspicuous. Imaging studies are often inconclusive. Therefore, diagnosing a TCS may prove difficult in some cases.
In this regard, Tubbs et al. [6–8] made the interesting observation that the lumbosacral angle (LSA) increases in children with (lipo)myelomeningocele at the time symptoms of TCS deteriorate. They suggested that the LSA as an objective tool may aid the clinician to determine if the spinal cord is symptomatically tethered, and if surgical untethering is needed. The aim of our study was to validate the findings of Tubbs et al in a consecutive cohort of children with different types of spinal dysraphism. Our initial goal was to validate the hypothesis that the LSA increases in children with spinal dysraphism who present with progressive symptoms and signs of TCS, and if so, to determine for which different types and/or levels of spinal dysraphism the LSA would be a valid indicator of progressive TCS. A secondary goal was to evaluate the influence of surgical untethering and eventual retethering on the LSA.
Patients and methods
Definition of TCS
There clearly is some inconsistency in the literature with regard to the definition of tethered cord and TCS. Therefore, we want to clearly state our definition of TCS in the context of spinal dysraphism as used in this article. Because some symptoms and signs of TCS may already be present at birth [9], some may worsen over time, and some may newly develop, we propose the following definition: neurologic, urologic, orthopaedic and/or gastrointestinal symptoms and signs supposedly due to abnormal tension on the spinal cord, which are (a) already present at birth, and have not changed during development, growth or maturation, or (b) already present at birth, and worsen during development, growth or maturation, or (c) not present at birth, and become clinically apparent during development, growth or maturation. Importantly, we consider TCS to be clinically progressive only if criteria described under (b) or (c) are fulfilled.
Study group inclusion/exclusion criteria
We retrospectively analyzed the magnetic resonance imaging (MRI) studies on all children (n = 115) from the Maastricht University Medical Center spina bifida database.
Inclusion criteria were age between 0 and 18 years, and availability of at least two sagittal MRI studies, including one study obtained in the postnatal period, one study obtained at the time symptoms of TCS deteriorated and the decision was made to operate, and (whenever available) one study obtained 2 to 3 years postoperatively. Whenever a child demonstrated symptoms and signs of progressive TCS (category b and c) after a previous untethering operation, imaging studies from this retethering episode were analyzed as well. Finally, whenever a child remained clinically stable, the most recent imaging study was analyzed.
Exclusion criteria were severe deformity of the caudal part of the spinal column (because of aberrant angles and/or the impossibility to measure the LSA), and for obvious reasons caudal regression syndrome (sacral agenesis). The former group of children included those with congenital lumbar kyphosis or kyphoscoliosis, as well as those with severe forms of spinal dysraphism who developed pronounced (kypho)scoliosis which made LSA measurements difficult or even impossible.
Control group
Because little is known about the LSA, we decided to analyze the MRI studies conducted on a control group as well. These were all children diagnosed with medulloblastoma, in whom the neuraxis had been screened for spinal metastases. Children with metastatic disease were included only if their spinal cord was not compressed, as cord compression may mimic a tethering mechanism. Again, at least two sagittal MRI studies had to be available. Children for this control group were included from our center as well as the University Medical Center Groningen and the Erasmus University Medical Center Rotterdam.
Data collection
In the Maastricht University Medical Center, children with spinal dysraphism are followed by a multidisciplinary spina bifida team. Most children undergo operation when their TCS is clinically progressive (category b and c); however, some children and especially those with a split cord malformation or a dermal sinus tract are operated on prophylactically. Whenever the spina bifida team suspects a progressive TCS, full spine MRI and urological studies as needed are performed.
After approval from the Medical Ethical Committee and Board of Directors of our center, we reviewed the children’s medical records for sex, age, type of spinal dysraphism, level of spinal dysraphism, ambulatory status, symptoms and signs indicative for TCS, surgical untethering, and symptoms and signs indicative for retethering. We divided their symptoms and signs into four categories as mentioned in the introduction (neurologic, urologic, orthopaedic and gastrointestinal). Finally, we reviewed the medical records of children with medulloblastoma for sex, age, local or metastatic disease, and spinal cord compression.
LSA measurements
The LSA was determined by the intersection of two straight lines drawn on a sagittal MRI of the lumbosacral region obtained in the supine position. We decided not to use plain radiographs because of another position (sitting or standing) during image acquisition, which may influence the LSA. The lines determining the LSA are the following: a line drawn perpendicular to a line tangential to the anterior surface of the body of the third lumbar vertebra, and a line drawn perpendicular to the sacral line, which is drawn by joining the middle of the anterior border of the body of the first sacral vertebra with that of the second sacral vertebra [6, 10] (Fig. 1).
Lumbosacral angle (LSA). The LSA is formed by two lines: a line drawn perpendicular to a line tangential to the anterior surface of the body of the third lumbar vertebra, and a line drawn perpendicular to the sacral line, which is drawn by joining the middle of the anterior border of the body of the first sacral vertebra with that of the second sacral vertebra. (Reprinted with permission from Dr. R. Shane Tubbs et al. and S. Karger AG, Basel [6])
The LSA was determined using a set triangle and/or a goniometer. Each LSA was measured twice by one of the authors (FR). Some measurements, most frequently from difficult cases with severe spinal deformity, were discussed with an orthopaedic surgeon specialized in scoliosis surgery (LvR). Importantly, to determine interobserver agreement, 46 LSA measurements were repeated by one of the co-authors (JV). Intra- and interobserver agreement were scored using kappa statistics.
Finally, we propose the following terms to identify the LSA measurements at different moments in time: initial LSA (first measurement), subsequent LSA (second measurement), LSA change (subsequent LSA minus initial LSA), preoperative LSA (preoperative) and postoperative LSA (postoperative).
Data analysis
Data are reported as mean (±SD) and median (range). Statistical analysis was performed using SPSS software version 15.0 for Windows. Because the data contained ordinal and interval variables in small sample sizes, we tested significance by parametric tests (analysis of variance (ANOVA), paired and unpaired t-tests), and nonparametric tests (Kruskal–Wallis test and Mann–Whitney U-test). P values less then 0.05 were considered statistically significant.
Results
Unfortunately, as many as 82 children from the cohort of 115 children in our spina bifida database were excluded from the study (Fig. 2), the reason almost invariably being that the original MRI hardcopies were missing. The remaining 33 children (19 boys, 14 girls) were included (Table 1). Their mean age at initial LSA measurement was 4 months (SD = 10 months). The underlying dysraphic disorder was a myelomeningocele in 20 patients (60%), a tight filum in six patients (18%), a lipoma in three patients, a Currarino syndrome in two patients, a split cord malformation in one patient and a meningocele in one patient. The level of spinal dysraphism was thoracic in two, thoracolumbar in four, lumbar in 12, lumbosacral in 13, and merely sacral in the remaining two.
Flow chart illustrating the selection process. *Reason for exclusion: deceased (n = 1), length of follow-up <10 months (n = 6), severe spinal deformity (n = 3). ** Reason for exclusion: original hardcopies unavailable (n = 56), clinically progressive TCS without previous images being available (n = 4)
Seven children (21%) were clinically stable with a mean interval between LSA measurements of 58 months (SD = 41 months) (Table 2). This group included four myelomeningoceles, one Currarino syndrome, one split cord malformation, and one lipoma. Of note, the latter two children were operated on prophylactically. Twenty-six children (79%) were clinically progressive. This group presented with their first progressive tethering episode at a mean age of 68 months (SD = 44 months) (Table 2). Finally, retethering occurred in three children, and a second retethering in two.
The control group (24 boys, nine girls) included one suprasellar and 32 posterior fossa medulloblastomas. Eleven children (33%) had metastatic disease, most often spinal leptomeningeal spread. The mean age at initial LSA measurement was 95 months (SD = 42 months), and the mean interval between LSA measurements was 42 months (SD = 31 months) (Table 1).
LSA measurements intra- and interobserver agreement
Kappa statistics for LSA measurements showed high intraobserver agreement (unweighted kappa 0.736, kappa with quadratic weighting 0.918) as well as interobserver agreement (unweighted kappa 0.588, kappa with quadratic weighting 0.872) (data not shown).
LSA in study and control group
Initial LSA in children with spinal dysraphism ranged from 21.5° to 64.0° (median 40.0°, mean 40.3°), subsequent LSA ranged from 37.0° to 89.0° (median 60.0°, mean 61.3°), and LSA change ranged from −5.5° to 57.5° (median 20.5°, mean 21.0°) (Table 3). Initial LSA in the control group ranged from 43.5° to 79.5° (median 60.0°, mean 61.5°), subsequent LSA ranged from 47.0° to 83.5° (median 64.0°, mean 64.0°), and LSA-change ranged from −10.5° to 19.0° (median 2.5°, mean 3.1°) (Table 3). Thus, initial LSA was smaller and LSA change was bigger for children with spinal dysraphism as opposed to the control group (both statistically significant with P values of <0.001). However, both groups were not age-matched, and when dividing both groups into comparable age categories, a significant difference was no longer observed (Table 4).
LSA in clinically progressive and clinically stable TCS
Initial LSA in children with progressive TCS ranged from 21.5° to 62.0° (median 41.0°, mean 40.4°), subsequent LSA ranged from 44.5 to 89.0° (median 60.0°, mean 61.1°), and LSA change ranged from −1.5° to 57.5° (median 22.3°, mean 20.6°) (Table 5). Initial LSA in children with stable TCS ranged from 21.5° to 64.0° (median 35.0°, mean 39.8°), subsequent LSA ranged from 37.0° to 89.0° (median 59.5°, mean 62.1°), and LSA change ranged from −5.5° to 52.5° (median 20.5°, mean 22.4°) (Table 5). Statistical analysis did not show a significant difference in LSA for children with clinically progressive TCS as opposed to clinically stable TCS, even when dividing both groups into comparable age categories (data not shown).
LSA in different types of spinal dysraphism
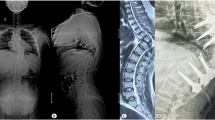
LSA measurements in different types of spinal dysraphism are listed in Table 6. Due to the small sample sizes (some subgroups included ≤2 individuals) we were unable to perform proper statistical analysis, however, the analyses we did perform (Kruskal–Wallis test and ANOVA without post hoc comparisons) did not show a significant difference in LSA measurements between different types of spinal dysraphism. Figure 3 illustrates LSA measurements in a girl with Currarino syndrome and a tight filum, whereas Fig. 4 illustrates LSA measurements in a girl with a myelomeningocele (both pre- and postoperatively).
LSA in different levels of spinal dysraphism
LSA measurements for different levels of spinal dysraphism (thoracic, thoracolumbar, lumbar, lumbosacral and sacral) are listed in Table 7. Statistical analysis did not show a significant difference in LSA measurements between these different levels.
LSA before and after surgical untethering
Twenty-six children were clinically progressive at some point and underwent surgical untethering. Postoperative MRI studies were available in 20 of these children, with a mean interval in between measurements of 30 months. Mean preoperative LSA was 62.6°, mean postoperative LSA was 67.8°. Thus, LSA increased after untethering with a statistically significant difference (P < 0.015) (Table 8). Retethering occurred in three children and a second retethering in two; however, because of very small sample sizes, we did not perform statistical analysis in these particular subgroups.
LSA in other subgroups
We observed no significant difference in LSA measurements in the study group between children with a normal gait, children with an impaired gait, children who walked late, and children who never learned to walk. Also, we observed no significant difference in LSA measurements between boys and girls, neither in the study nor in the control group. Finally, we observed no significant difference in LSA measurements for children in the control group with and without metastatic disease (data not shown).
Discussion
In this study, we analyzed the LSA in children with spinal dysraphism (clinically progressive TCS as opposed to clinically stable TCS), and in controls with medulloblastoma. When dividing these groups into comparable age categories, we observed no significant differences in LSA measurements.
Abitbol studied the LSA in 131 healthy children, including 62 boys and 69 girls [10]. The LSA (measured in subjects resting on their side) increased from an average of 20° at birth to an average of 70° at the age of 5 years, and remained stable thereafter. The LSA progressed at approximately the same rate for both sexes, and at the age of 11 months varied from 20° to 45°. Abitbol theorizes the LSA develops as a result of the acquisition of erect posture and the ontogeny of bipedal locomotion more than as a result of a generalized growth trend as manifested by increasing age, height, or weight. He observed that in children who were able to stand up and walk early, the LSA developed early, while in children who were slower to learn to stand or walk, the LSA developed and reached its final state later in life. Moreover, children who never learned to walk or had an impaired posture and gait because of a pathologic condition developed only a minimal LSA.
Tubbs et al. [6, 7] retrospectively analyzed the LSA in 30 children with a myelomeningocele and 25 children with a lipomyelomeningocele. They observed that the LSA was often increased for their age. Statistical analysis of symptomatic and asymptomatic children, i.e. clinically progressive and clinically stable children, demonstrated a mean LSA change of 18.85° and 6.69° (p = 0.0371) respectively for children with a myelomeningocele [6], and 13° and 5° (p = 0.0202) respectively for children with a lipomyelomeningocele [7].
There is little doubt that making a decision in favour of an untethering operation may sometimes be quite difficult even in the setting of an experienced spina bifida team. Based on the study by Tubbs et al. as mentioned above, we assumed that the LSA would increase in children at the time of progressive TCS. If so, the LSA would have been an objective indicator for progressive TCS. Our findings, however, do not support the earlier findings of Tubbs et al. Although LSA measurements in the first year of life in our study group were comparable to those of Tubbs et al., we did not observe a significant difference in LSA measurements for children with clinically progressive TCS as opposed to clinically stable TCS. Moreover, although LSA measurements in our control group were comparable to those observed by Abitbol [10] in healthy children, we did not observe a significant difference in final LSA development (expressed as subsequent LSA) in children with progressive TCS as opposed to the control group with medulloblastoma (Tables 3 and 5). The reasons for this discrepancy are unclear. One possible explanation may be the simultaneous use of more than one imaging modality by Tubbs et al., more specifically X-ray and MRI studies, whereas we used MRI studies exclusively. Also, the LSA may be measured more accurately on MRI studies because of their superior resolution. Interestingly, in contrast to the findings of Abitbol, we observed no differences for children with different ambulatory status (walking versus wheelchair bound). We therefore hypothesize that the LSA develops as a result of the acquisition of erect posture and the influence of gravity rather than as a result of bipedal locomotion.
The reader may have noted that the LSA change was larger in the study group than in the control group. He should realize, however, that initial measurements in the control group cannot be compared to initial measurements in the study group, because mean age at initial measurement was 95 months in the control group as opposed to 4 months in the study group. When dividing both groups into comparable age categories, a significant difference in LSA measurements was no longer observed. As pointed out by Abitbol, it is the natural course of the LSA to increase in the first 5 years of life. Therefore, the difference in LSA change between study and control group is explained by the different age distribution of the children, implying a different stage of LSA maturation. This also explains the observed increase in postoperative LSA (67.8°) compared to preoperative LSA (62.6°): the LSA does not change in children with progressive TCS but merely follows its natural course.
Study limitations and future perspectives
We used the same method used by as Abitbol [10] and Tubbs et al [6] in measuring the LSA. To the best of our knowledge, this method has never been validated; however, intra- and interobserver agreement in our study were high, suggesting the method is valid at least for this group of children. As mentioned above, this method is not suitable for severe (kypho)scoliosis that may be affecting children with severe spinal dysraphism. Three children were excluded for this reason.
Unfortunately, as many as 82 children from the cohort of 115 children in our database were excluded, the reason almost invariably being that the original MRI hardcopies were missing. Some subgroups (e.g. different types of spinal dysraphism, different levels of spinal dysraphism) were too small (n ≤ 2) to perform statistical analysis. However, we do not believe this influenced our overall conclusion.
Ideally, the control group should have been obtained by random selection of healthy, non-hospitalized, age-matched children; however, we did not take this option because of ethical considerations and costs. Therefore, we chose children with medulloblastoma, excluding those with metastatic spinal cord compression which may mimic a tethering mechanism. For obvious reasons, imaging obtained in the postnatal period was unavailable in these children. Finally, conflicting findings in this study as compared to those obtained by Tubbs et al (both retrospective) may warrant a prospective study with healthy, age-matched controls.
Conclusion
We did not observe significant differences in LSA measurements in children with clinically progressive TCS as opposed to clinically stable TCS. Therefore, the LSA does not help the clinician to determine if there is significant spinal cord tethering, nor if surgical untethering is needed.
References
Bui CJ, Tubbs RS, Oakes WJ (2007) Tethered cord syndrome in children: a review. Neurosurg Focus 23:1–9
Lew SM, Kothbauer KF (2007) Tethered cord syndrome: an updated review. Pediatr Neurosurg 43:236–248
Yamada S, Won DJ, Yamada SM (2004) Pathophysiology of tethered cord syndrome: correlation with symptomatology. Neurosurg Focus 16:E6
Michelson DJ, Ashwal S (2004) Tethered cord syndrome in childhood: diagnostic features and relationship to congenital anomalies. Neurol Res 26:745–753
Steinbok P, MacNeily AE (2007) Section of the terminal filum for occult tethered cord syndrome: toward a scientific answer. Neurosurg Focus 23:1–4
Tubbs RS, Wellons JC 3rd, Bartolucci AA, Blount JP, Oakes WJ (2002) Horizontal sacrum as an indicator of a tethered spinal cord. Pediatr Neurosurg 36:209–213
Tubbs RS, Naftel RP, Rice WC, Liechty P, Conklin M, Oakes WJ (2006) The patient with symptoms following resection of a lipomyelomeningocele: do increases in the lumbosacral angle indicate a tethered spinal cord? J Neurosurg 105(1 Suppl):62–64
Tubbs RS, Bui CJ, Loukas M, Shoja MM, Oakes WJ (2007) The horizontal sacrum as an indicator of the tethered spinal cord in spina bifida aperta and occulta. Neurosurg Focus 23:1–4
Beuls EA, Vanormelingen L, van Aalst J, Vandersteen M, Adriaensen P, Cornips EM et al (2003) In vitro high-field magnetic resonance imaging-documented anatomy of a fetal myelomeningocele at 20 weeks’ gestation. A contribution to the rationale of intrauterine surgical repair of spina bifida. J Neurosurg 98(2 Suppl):210–214
Abitbol MM (1987) Evolution of the lumbosacral angle. Am J Phys Anthropol 72:361–372
Conflict of interest
The authors declare that they have no conflict of interest.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
Erwin M. J. Cornips and Femke G. E. M. Razenberg contributed equally to this article.
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Cornips, E.M.J., Razenberg, F.G.E.M., van Rhijn, L.W. et al. The lumbosacral angle does not reflect progressive tethered cord syndrome in children with spinal dysraphism. Childs Nerv Syst 26, 1757–1764 (2010). https://doi.org/10.1007/s00381-010-1281-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-010-1281-0