Abstract
Methionine is an indispensable sulfur amino acid that functions as a key precursor for the synthesis of homocysteine and cysteine. Studies in adult humans suggest that splanchnic tissues convert dietary methionine to homocysteine and cysteine by means of transmethylation and transsulfuration, respectively. Studies in piglets show that significant metabolism of dietary indispensable amino acids occurs in the gastrointestinal tissues (GIT), yet the metabolic fate of methionine in GIT is unknown. We show here that 20% of the dietary methionine intake is metabolized by the GIT in piglets implanted with portal and arterial catheters and fed milk formula. Based on analyses from intraduodenal and intravenous infusions of [1-13C]methionine and [2H3]methionine, we found that the whole-body methionine transmethylation and remethylation rates were significantly higher during duodenal than intravenous tracer infusion. First-pass splanchnic metabolism accounted for 18% and 43% of the whole-body transmethylation and remethylation, respectively. Significant transmethylation and transsulfuration was demonstrated in the GIT, representing ≈27% and ≈23% of whole-body fluxes, respectively. The methionine used by the GIT was metabolized into homocysteine (31%), CO2 (40%), or tissue protein (29%). Cystathionine β-synthase mRNA and activity was present in multiple GITs, including intestinal epithelial cells, but was significantly lower than liver. We conclude that the GIT consumes 20% of the dietary methionine and is a significant site of net homocysteine production. Moreover, the GITs represent a significant site of whole-body transmethylation and transsulfuration, and these two pathways account for a majority of methionine used by the GITs.
Keywords: cystathionine β-synthase, homocysteine, intestine
The sulfur amino acids, methionine, homocysteine, and cysteine, have attracted considerable interest in the last decade. Methionine is an indispensable amino acid and is transmethylated intracellularly to homocysteine via S-adenosylmethionine (SAM), an important methyl donor for most biological methylation reactions (1). Homocysteine can be further catabolized to cysteine through transsulfuration, which is regulated by the enzymes cystathionine β-synthase (CBS) (EC 4.2.1.22) and cystathionine γ-lyase (EC 4.4.1.1). Homocysteine can also be used for methionine synthesis through remethylation. Consequently, homocysteine represents a critical regulatory control point for methionine and cysteine synthesis and folate metabolism.
Homocysteine is normally present in human plasma at low concentrations. However, elevated plasma homocysteine concentrations have important implications for human health and disease. Clinical studies indicate that hyperhomocysteinemia is strongly associated with increased risk of cardiovascular disease, with ischemic and hemorrhagic stroke in infants and children (2–4), and, more recently, Alzheimer's disease and other neurological diseases in adults (5). Genetic defects in methionine metabolism related to methionine synthase, N5,10-methylene-tetrahyrdofolate, also result in neural dysfunction, mental retardation, and pregnancy complications (6–8). Recent studies have linked homocysteine, folate, and DNA methylation with gastrointestinal diseases, namely inflammatory bowel disease and colon cancer (9–13). The underlying mechanism linking homocysteine to inflammatory disease may be the induction of leukocyte adhesion molecules and proinflammatory cytokines in vascular endothelial cells (10).
Methionine is also a precursor for cysteine, which plays a key role in cellular protein function and redox status by virtue of its thiol (−SH) moiety. In addition, it also serves as a precursor of glutathione, a major cellular antioxidant, as well as CoA, taurine, and inorganic sulfur. Several tissues in the body are capable of cysteine synthesis (14), which is why cysteine is considered nutritionally dispensable. However, increasing evidence that oxidant stress is linked to many disease pathologies and aging has focused attention on the antioxidant functions of cysteine and its product, glutathione, leading some to suggest that cysteine is a conditionally indispensable dietary nutrient (15–17).
Most cells in the body are capable of transmethylation and remethylation, yet homocysteine metabolism via transsulfuration seems limited to certain tissues. Early studies by Mudd et al. (18) showed that CBS and cystathionine γ-lyase are active mainly in human liver tissue, and to a lesser extent, in extra hepatic tissues including pancreas, kidney, small intestine, brain, and lung. Stegink and den Besten (19) first reported in vivo evidence to implicate splanchnic tissues as a key site of methionine transsulfuration by demonstrating that plasma cysteine concentrations are significantly higher in human subjects fed a methionine-containing, cystine-free diet enterally versus intravenously. However, subsequent metabolic studies with stable isotopic tracers also have indirectly suggested that a substantial fraction of the dietary methionine undergoes transmethylation and remethylation during first-pass splanchnic metabolism in adult humans (20, 21). More recent studies show that the whole-body methionine requirement and circulating homocysteine concentrations are significantly higher in piglets fed enterally than parenterally, demonstrating that splanchnic methionine metabolism is nutritionally significant (22, 23).
Despite the clear evidence that splanchnic tissues play a major role in methionine transmethylation and transsulfuration, the relative contribution of the gastrointestinal tissues (GIT) remains unclear. Our previous studies have shown that GIT extensively metabolize dietary indispensable amino acids, namely lysine, threonine, and leucine (24–26). In the case of methionine, our studies and those of others suggest that substantial metabolism and even oxidation of dietary methionine occurs in the gut (26, 27). However, the extent of transmethylation and transsulfuration in the GIT and its relative contribution to whole-body methionine metabolism has not been established. In this report, we have coupled our piglet model of arteriovenous balance across the GIT with an established stable isotopic tracer approach using [1-13C and methyl-2H3]methionine to investigate the metabolic fate of methionine in the gut and the contribution to the whole-body rates of transmethylation and transsulfuration. We hypothesized that there is substantial transmethylation, transsulfuration, and remethylation of dietary methionine by GIT and that dietary rather than systemically derived methionine is preferentially metabolized.
Results
Whole-Body Methionine Metabolism.
Mean weight of the animals on the first and second days of the experiment were 6.74 ± 1.89 kg and 7.52 ± 1.99 kg, respectively. No significant differences between intravenous (IV) and intraduodenal (ID) infusions were observed in mean whole-body CO2 production (IV 46.55 ± 1.16 mmol·kg−1·h−1 and ID 45.50 ± 0.97 mmol·kg−1·h−1) and CO2 production by the portal drained viscera was 6.95 ± 0.57 mmol·kg−1·h−1 IV and 6.73 ± 0.55 mmol·kg−1·h−1 ID.
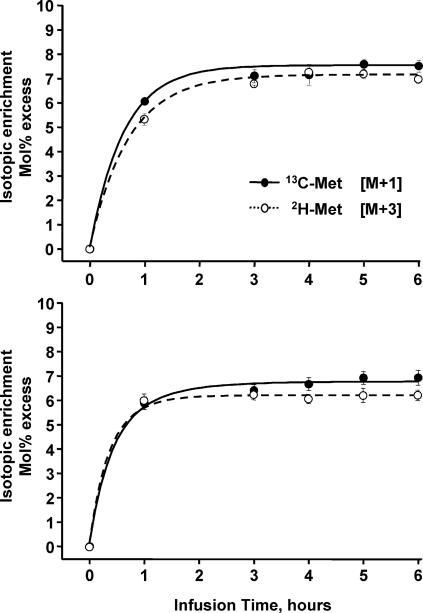
As shown in Fig. 1, steady-state of plasma isotopic enrichment (expressed as mole percent excess, MPE) of [1-13C]methionine and [2H3]methionine was achieved after 5 h during both infusion modes. Methionine plateau was defined as the mean plasma enrichment between 5 and 6 h. Steady-state of [1-13C]homocysteine was not achieved after 6 h of infusion (data not shown), and these values were not used to estimate the tissue intracellular precursor enrichment for whole-body fluxes as done previously (28). However, the plasma [1-13C]homocysteine enrichments were used to calculate methionine kinetics in the GIT, because the assumption of steady-state is not necessary. Whole-body methionine kinetics are depicted in Table 1, and rates are expressed as μmol·kg−1·h−1. Whole-body methionine transmethylation, remethylation, and incorporation into protein synthesis were significantly (P < 0.05) higher during ID than IV tracer infusion, indicating first-pass splanchnic metabolism. Whole-body transmethylation represented 25% and 27% of methionine flux when infused IV and ID, respectively. Whole-body transsulfuration represented 21% and 20% of methionine flux when infused IV and ID, respectively, and was not significantly different between the infusion groups. Most of whole-body methionine flux (≈80%) was used for protein synthesis and only ≈20% was metabolized through transmethylation and transsulfuration.
Fig. 1.
Time course of mean plasma tracer enrichments during IV (Upper) and ID (Lower) infusion of [1-13C]methionine (filled circles) and [methyl-2H3]methionine (open circles). Enrichments expressed as mole percent excess (MPE). Means ± SE (n = 16).
Table 1.
Whole-body methionine kinetics
| IV | ID | |
|---|---|---|
| [Methyl-2H3]methionine flux | 130 ± 4 | 147 ± 2* |
| [1-13C]methionine flux | 122 ± 3 | 133 ± 2* |
| Transmethylation | 33 ± 3 | 40 ± 3† |
| Transsulfuration | 26 ± 2 | 26 ± 2 |
| Remethylation | 8 ± 1 | 14 ± 1* |
| Protein synthesis | 97 ± 3 | 107 ± 2† |
Data are mean ± SE (n = 16). Rates are expressed as μmol·kg−1·h−1 for IV and ID tracer administration.
*P < 0.01 IV vs. ID.
†P < 0.05 IV vs. ID.
Methionine Metabolism in the GIT.
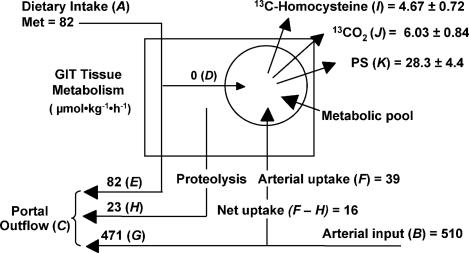
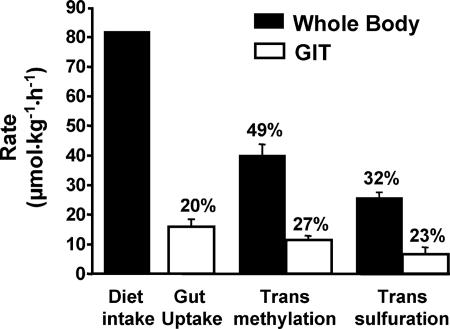
Methionine kinetics of the GIT are shown in Table 2 and Fig. 2. Total net methionine utilization by the GIT accounted for 20% of the dietary methionine intake. However, there was no first-pass metabolism of dietary methionine in the GIT. After correction for recycling and arterial uptake of ID methionine tracer absorbed into the portal blood, the net methionine uptake was 16 μmol·kg−1·h−1, indicating that the GIT preferentially metabolized systemic methionine rather than dietary methionine. Release of [13C]homocysteine and 13CO2 by the GIT, which is a reflection of transmethylation, accounted for 67% of the GIT [13C]methionine uptake. Transsulfuration was measured as the 13CO2 release by the portal drained viscera, which was 38% of the [13C]methionine uptake by the GIT. The contribution of GIT to whole-body metabolism is shown in Fig. 3. The rate of GIT methionine uptake represented 20% of the dietary methionine intake, whereas ≈49% and 32% of the dietary methionine intake was metabolized in the whole body via transmethylation and transsulfuration, respectively. The GIT represented 27% and 23% of whole-body rates of transmethylation and transsulfuration, respectively.
Table 2.
Steady-state methionine and homocysteine concentrations and isotopic enrichments in plasma and tissue
| IV | ID | |
|---|---|---|
| Arterial methionine | ||
| Concentration, μM | 202 ± 9 | 200 ± 8 |
| [1-13C]methionine, MPE | 7.56 ± 0.19 | 6.94 ± 0.09 |
| [Methyl-2H3]methionine, MPE | 7.05 ± 0.17 | 6.25 ± 0.08 |
| Portal methionine | ||
| Concentration, μM | 208 ± 16 | 210 ± 17 |
| [1-13C]methionine, MPE | 6.37 ± 0.16 | 7.75 ± 0.24 |
| [Methyl-2H3]methionine, MPE | 5.97 ± 0.15 | 7.19 ± 0.22 |
| Arterial homocysteine | ||
| Concentration, μM | 7.80 ± 0.91 | 6.54 ± 0.48 |
| [1-13C]homocysteine, MPE | 5.60 ± 0.19 | 5.52 ± 0.11 |
| Portal homocysteine | ||
| Concentration, μM | 8.48 ± 0.76 | 8.16 ± 0.57 |
| [1-13C]homocysteine, MPE | 5.58 ± 0.19 | 5.63 ± 0.10 |
| Intestine [1-13C]methionine, MPE | 3.25 ± 0.29 | 3.07 ± 0.48 |
| Intestine [methyl-2H3]methionine, MPE | 0.34 ± 0.03 | 0.38 ± 0.09 |
| Liver [1-13C]methionine, MPE | 4.34 ± 0.16 | 3.79 ± 0.16 |
| Liver [methyl-2H3]methionine, MPE | 0.24 ± 0.01 | 0.20 ± 0.01 |
Data are mean ± SEM (n = 16 plasma and n = 6–8 tissues) for IV and ID tracer administration.
Fig. 2.
Schematic representation of the metabolic fate of enteral and systemic methionine kinetics in the GIT (n = 16). Dietary methionine intake (A); arterial methionine flux through the GIT (B); portal methionine outflow (C); unidirectional, first-pass uptake of dietary methionine by the GIT (D); dietary methionine not metabolized by the GIT in first pass (E); unidirectional uptake of arterial methionine by the GIT (F); arterial methionine not metabolized by the GIT (G); recycled methionine derived from proteolysis (H); and methionine that is converted to homocysteine (I), CO2 (J), and protein (K) by the GIT. Rates expressed as μmol·kg−1·h−1. Dietary intake includes [1-13C] and [methyl-2H3]methionine tracers. Detailed explanation of equations and assumptions used for calculating the methionine kinetic in the GIT are included in supporting information (SI) Appendix.
Fig. 3.
The absolute rates and relative proportions of dietary methionine intake, transmethylation, and transsulfuration in the whole body (filled bars) and GIT (open bars). Rates expressed as μmol·kg−1·h−1. Percentages above filled bars represent whole-body rates relative to dietary methionine intake, whereas those above open bars represent GIT rates relative to the respective whole-body rates. Means ± SE (n = 16).
The isotopic enrichments of free [1-13C] and [methyl-2H3]methionine in the intestinal and liver tissues were not different between IV and ID groups (Table 2). However, the enrichment of [2H3]methionine was significantly (P < 0.01) lower than [13C]methionine in both the intestine (ratio [2H3]methionine/[13C]methionine = 0.12) and liver (ratio [2H3]methionine/[13C]methionine = 0.05); the ratio of [2H3]methionine/[13C]methionine was significantly (P < 0.001) lower in the liver than intestine. This relationship also was observed for protein-bound [13C]methionine and [2H3]methionine in the intestinal and liver tissue (data not shown). The net portal fluxes of methionine, homocysteine, and CO2 are shown in Table 3. Consistent with tracer flux, the net rate of methionine absorption from the GIT was 78% and 82% of the dietary intake in IV and ID groups, respectively. The net homocysteine flux was significantly positive, indicating net production by the GIT; the homocysteine flux represented 20–25% of the respective GIT methionine utilization rate.
Table 3.
Dietary methionine intake and net portal fluxes of methionine, homocysteine, and CO2
| IV | ID | |
|---|---|---|
| Enteral methionine intake | 62 | 82 |
| Portal plasma flow (liter·kg−1·h−1) | 2.58 ± 0.16 | 2.44 ± 0.12 |
| Net portal methionine absorption | 48 ± 3 | 67 ± 3 |
| Methionine intake, % | 78 ± 4 | 82 ± 3 |
| Net portal methionine utilization | 14 ± 3 | 15 ± 3 |
| Methionine intake, % | 22 ± 4 | 18 ± 3 |
| Net portal homocysteine release | 2.7 ± 0.5 | 3.9 ± 0.5 |
| Portal methionine uptake, % | 20 ± 3 | 25 ± 4 |
| Net portal CO2 release | 6,948 ± 226 | 6,725 ± 204 |
Data are mean ± SE (n = 16). Rates are expressed as μmol·kg−1·h−1 except where indicated.
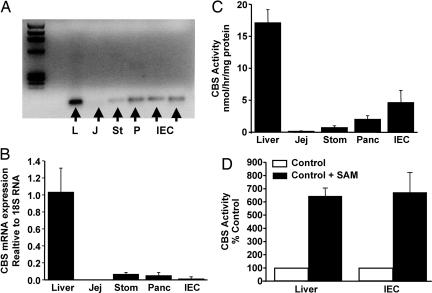
The mRNA expression and activity of CBS in various GI tissues are expressed in Fig. 4. A single PCR product of 76 bp derived from a sequence spanning exons 6 and 7 of the porcine CBS gene was measured in all tissues (Fig. 4A). The relative expression of CBS mRNA in liver tissue was >10-fold higher than in any GI tissue measured. However, the CBS activity in liver tissue was only 3- to 5-fold higher than in GITs. Interestingly, both liver and intestinal epithelial cell CBS activity was markedly (≈6-fold) increased above the basal rate by coincubation with 1.0 mM SAM, a known allosteric activator of the enzyme (28).
Fig. 4.
CBS mRNA abundance and enzymatic activity in liver and selected GITs. (A) The relative amounts of CBS mRNA product derived from 100 ng of RNA of representative tissue samples from liver (L), jejunum (J), stomach (St), pancreas (P), and intestinal epithelial cells (IEC) after RT-PCR and separation on agarose gel. (B) Abundance of CBS mRNA expressed relative to 18S RNA in liver, jejunum, stomach, pancreas, and IEC (n = 4). (C) CBS enzymatic activity determined in liver, jejunum, stomach, pancreas, and IEC (n = 4). (D) Relative changes in CBS enzymatic activity determined in liver tissue and intestinal epithelial cells in the absence and presence of 1.0 mM SAM (n = 3). Means ± SEM.
Discussion
The main objective of this study was to quantify the metabolic fate of methionine in the GIT by using our established in vivo model coupling organ balance and isotopic tracer kinetics. Our results demonstrate in vivo that the GIT is a metabolically significant site of methionine transmethylation and transsulfuration. Moreover, we show in vivo evidence that the GIT is not only a site of intracellular homocysteine synthesis but also of net release into the circulation. This finding provides evidence for the metabolic role of the GIT in the etiology of homocysteinemia and how this may be impacted by gastrointestinal disease states. This study also extends our previous work with other indispensable amino acids, e.g., lysine, leucine, threonine, and phenylalanine, and shows that, in addition to the liver, the GIT is an active site of methionine metabolism in the body (24–26, 29, 30).
Our results indicated that the GIT metabolize ≈20% of the dietary methionine intake. Recent studies in neonatal piglets fed cysteine-free diets demonstrated that the whole-body methionine requirement is ≈40% lower in total parenterally fed (TPN) compared with enterally fed pigs (31). The difference in this case was attributed to GIT metabolism, because TPN bypasses the gut and results in gut atrophy. A subsequent study showed that feeding an excess of dietary cystine significantly decreased the methionine requirement consistent with the methionine-sparing effect of cysteine (22). However, even with excess dietary cystine, the methionine requirement in TPN-fed pigs was still ≈28% lower than enterally fed pigs, again implying that the GIT represents 28% of body methionine metabolism. The latter study is comparable to our current study where dietary cystine was in excess of the methionine intake. The difference between our direct estimate of 20% and the indirect estimate of 28% GIT metabolism could be due to the nature and composition of the diets (formula versus elemental diet) or that our pigs were slightly older (4 versus 1 week old).
The finding of significant transmethylation and transsulfuration in the GIT is supported by previous reports and our current evidence showing the presence of enzymes involved in methionine metabolism in stomach, pancreas, and intestinal epithelial cells (18, 32). Recent evidence from colonic cell (Caco-2) culture studies also showed the presence of methionine transmethylation and transsulfuration activity (33). The finding of net homocysteine production potentially implicates the gut in homocysteinemia. It also explains why enteral nutrition results in significantly higher circulating homocysteine concentrations than TPN (23). A striking observation was the significant reduction in the tissue-free enrichment of [2H3]methionine compared with [13C]methionine; the mean ratio of [2H3]methionine/[13C]methionine was 0.05 in liver and 0.12 in intestine. These ratios are explained by the high rate of intracellular methylation and necessary loss of the deuterated methyl moiety via SAM synthesis. This indicates a substantial methylation rate in the intestine that is nearly half of that observed in the liver. It is important to note that the current estimates of methionine transmethylation and transsulfuration are minimal estimates, given the generous dietary cystine intake, and are likely higher under conditions of cysteine and folate deficiency or oxidant stress. Yet, it is remarkable that despite the high dietary cysteine intake, the GIT represent ≈23% of whole-body transsulfuration and a third of all methionine used by the gut was used for cysteine synthesis. This value is nearly twice as high as that reported recently for sheep, where they observed that ≈10% of whole-body methionine oxidation occurred in GIT (27). It is of interest that isolated epithelial cells had the highest CBS activity among the GI tissues measured. Oxidant stress is known to increase methionine transsulfuration to meet the increased cysteine demand for cellular glutathione synthesis (34, 35). This suggests that the metabolic requirement for methionine and cysteine by the gut may be increased in conditions such as inflammatory bowel disease and enteric infection.
We observed substantially higher whole-body rates of transmethylation (3-fold) and transsulfuration (6-fold) in our young pigs when compared with those reported in adult humans (21). Moreover, when expressed as fraction of transmethylation, we found that most of the body homocysteine produced in young pigs is metabolized via transsulfuration, and less is remethylated when compared with adult humans; it is unclear whether this is due to difference in species or age. A particularly important finding was that the whole-body transmethylation and remethylation rates were significantly higher during the enteral compared with the IV tracer infusion protocol. This suggests that nearly 18% and 43% of the whole-body transmethylation and remethylation, respectively, occurs in first-pass by splanchnic tissues. However, another key observation from this study was that the GIT preferentially utilizes methionine from the arterial circulation rather than the diet, contrary to our hypothesis. Thus, the results indicate that the preferential first-pass splanchnic metabolism of dietary methionine occurs in the liver and not the GIT. These findings are consistent with our evidence of substantial intracellular methylation rates in both the liver and intestinal tissues. Moreover, our findings support indirect evidence from separate clinical studies where a dual-labeled [1-13C-methyl-2H3]methionine tracer was given intravenously and orally (20, 21). The authors of these two studies estimated that there is no first-pass splanchnic metabolism when based solely on kinetics of the [1-13C-methyl-2H3]methionine isotopomer. However, these authors found that the enrichment of [1-13C]methionine isotopomer was considerably higher when the [1-13C-methyl-2H3]methionine tracer was given orally than after IV infusion, indicating the presence of significant first-pass splanchnic transmethylation and remethylation of dietary methionine. Recent in vivo studies in sheep also indicate that the liver and gut tissues are important sites of homocysteine remethylation (36). The markedly lower enrichment of the [methyl-2H3]methionine compared with [1-13C]methionine implies a very high fractional rate of methylation and remethylation. Therefore, our results together with previous reports in humans and sheep strongly suggest that the GIT and liver are major sites of homocysteine remethylation.
In this study, the relative plasma [13C]homocysteine/[13C]methionine enrichments were considerably higher than recent reports in humans under postabsorptive (37, 38) and insulin-stimulated conditions. Theoretically, in tissues with the enzymatic capacity for transmethylation the intracellular enrichment of [13C]methionine and [13C]homocysteine should be similar, assuming that there is one common intracellular pool. Although we did not measure tissue [13C]homocysteine enrichments, the tissue [13C]methionine enrichment in the intestine (3.07 MPE) and liver (3.79 MPE) was significantly lower than that of plasma [13C]homocysteine (5.52 MPE). The plasma [13C]homocysteine enrichment theoretically represents the summation of transmethylation in the whole body. These results further suggest that the fractional rates of methionine transmethylation to homocysteine are disproportionately higher in the liver and GIT compared with other tissues in the body.
In conclusion, this study provides in vivo kinetic evidence for methionine transmethylation and transsulfuration in the developing GIT. Moreover, we show the GIT to be a site of net homocysteine release into the circulation. The high rates of transmethylation in the GIT may be functionally linked to methyl demand for synthesis of polyamines, phosphatidylcholine, or creatine (39). The GIT consumed 20% of the dietary methionine intake and approximately two-thirds of this was used for synthesis of homocysteine and cysteine. We also show that the GIT contributes significantly to whole-body methionine transsulfuration and that CBS expression is localized to epithelial cells within the small-intestinal mucosa. We speculate that the high rate of methionine transsulfuration in the GIT is driven by cysteine needs for glutathione synthesis because of the oxidant stress associated with the high metabolic activity of proliferating epithelial cells. Another demand for intestinal methionine transsulfuration may be for synthesis of cysteine-rich mucins secreted by goblet cells involved in innate immune function (40). We also found significant first-pass splanchnic transmethylation and remethylation, but this appears to be confined only to the liver, because there was no first-pass methionine use by the GIT. Taken together, the results suggest that the GIT is a key site for regulation of homocysteine metabolism via dietary and other means. These studies also suggest that GI disease states may play a role in the development and treatment of hyperhomocysteinemia or conversely that dysregulation of gut homocysteine metabolism may contribute to pathologies of GI diseases, namely inflammatory bowel disease.
Materials and Methods
Animals and Design.
The protocol was approved by the Animal Protocol Review Committee of Baylor College of Medicine and conformed to the U.S. Department of Agriculture guidelines. Sixteen, 14-day-old female piglets (Large White × Hampshire × Duroc) were adapted for 7 days to a liquid milk replacer diet (Litterlife; Merrick, Middleton, WI) that provided 25 g of lactose, 5 g of fat, and 12.5 g of protein per kg body weight daily. Methionine and cystine contents were 0.52% and 0.61%, respectively, providing a daily intake of 0.25 g methionine/kg and 0.31 g of cystine/kg. At 20 days of age, the piglets (n = 16) were surgically implanted with catheters as described (26, 41). One week after surgery, each piglet received ID and IV tracer infusions on two different days in a randomized, cross-over design with at least one day between the ID and IV infusions. To estimate whole-body CO2 production, a 2-h infusion of [13C]sodium bicarbonate was performed before the methionine tracer infusion (26).
Tracer Protocol.
At 27 days of age, piglets were fed a bolus meal supplying 1/12 of the preceding total intake after an overnight fast. Constant duodenal infusion at a rate of 1/24 of the daily intake (ml·kg−1·h−1) was started 1 h after the animal had consumed its meal; this was continued for 8 h. Immediately after starting the duodenal feeding, all piglets received a primed, continuous IV infusion (5 and 10 μmol·kg−1·h−1, respectively) of [13C]sodium bicarbonate (99% APE; Cambridge Isotope Laboratories, Andover, MA) for 2 h. At 120 min, the [13C]bicarbonate infusion ended, and an immediate infusion of [1-13C]methionine and [methyl-2H3]methionine (98% and 99% APE, respectively; Cambridge Isotope Laboratories) was administrated for 6 h either via the jugular (IV) or via the duodenal (ID) catheter. The primed, continuous infusion rate was 10 μmol·kg−1·h−1 for each methionine tracer, so the total isotopic methionine infusion rate was 20 μmol·kg−1·h−1. Arterial and portal blood samples were collected at 0, 90, 115, and 120 min and 6, 7, and 8 h. Portal blood flow was monitored continuously by transit-time ultrasound for 30 min before the initial formula feeding and throughout the entire 8-h protocol as described (24, 26). After tracer infusion on the second study day, animals were euthanized (Beutanasia-D; Schering-Plough Animal Health, Kenilworth, NJ) and intestinal, pancreas, stomach, and liver tissues were collected and frozen at −80°C.
Sample Preparation and Analysis.
Blood gases (Chiron Diagnostics, Halstead, Essex, U.K.) and hematocrit were determined immediately in all arterial and portal blood samples, and isotopic enrichment of 13CO2 in whole blood was analyzed by isotope ratio mass spectrometer as described (26). Plasma was obtained from arterial and portal blood, and an aliquot of plasma was combined with methionine sulfone (0.4 mM) and stored at −80°C until further amino acid analysis by HPLC (PicoTag System; Waters, Woburn, MA).
Measurement of Stable Isotope Tracer Enrichments.
Plasma isotopic enrichments of [1-13C]methionine, [methyl-2H3]methionine, and [1-13C]homocysteine were quantified on the heptafluorobutyric anhydride (HFBA) derivatives by GC-MS by using a modification of the methods described (37, 42). Blood 13CO2 enrichment was determined by gas isotope ratio mass spectrometry (26). Plasma homocysteine was determined by isotope dilution using D8-homocystine (37, 42). Briefly, plasma was acidified with 10% trichloroacetic acid, amino acids were separated by cation-exchange (AG 50W-X8; Bio-Rad, Richmond, CA), treated with DTT (DTT; Sigma–Aldrich, St. Louis, MO), and derivatized with HFBA (42). GC-MS was performed by negative chemical ionization on a GC-MS model HP-6890/5973 MSD (Hewlett–Packard, Palo Alto, CA). Ion abundance was monitored with selected-ion monitoring (SIM); mass-to-charge (m/z) for natural methionine [M + 0], [1-13C]methionine [M + 1], and [methyl-2H3]methionine [M + 3] were 367, 368, and 370, respectively. Ions were monitored by SIM at m/z 449–553 for natural homocysteine, [1-13C]homocysteine and D4-homocysteine. Isotopic enrichments of both tracers were expressed as mole percent excess (MPE), and the concentration of homocysteine was calculated by isotope dilution as described (37). The frozen small intestine (n = 16) and a liver sample were homogenized and separated into free and bound fractions by adding sulfosalicylic acid (6%) to precipitate protein. The tissue-free fraction was then subjected to cation exchange as described above, the eluant was dried under nitrogen, and derivatized by using ethylchloroformate. GC-MS analysis (Carlo Erba GC800 and Fisons MD800; Interscience BV, Breda, The Netherlands) was performed in electron-impact mode, and the ion abundance was monitored in SIM mode; m/z for natural methionine [M + 0], [1-13C]methionine [M + 1], and [2H3]methionine [M + 3] were 249, 250, and 252, respectively.
CBS Measurement.
Total RNA was isolated from the frozen porcine liver, jejunum, stomach, and pancreas samples and isolated jejunum cells by using RNeasy Mini kit (Qiagen, Valencia, CA). Approximately 100 ng of total RNA was used for each real-time qRT-PCR. Primers and probe designed from the porcine CBS mRNA (GenBank accession no. BP446783) were as follows: CBS forward primer (200 nM): CAGCGCTGCGTGGTGAT; CBS reverse primer (200 nM): CAGACTCTGTGCGCAACTACATGTCCAAG; and CBS TaqMan TAMRA probe (100 nM): 6FAM-GCAGCATCCACTTGTCACTCA-TAMRA. Primers and probe of ribosomal RNA (18S rRNA; Applied Biosystems, Foster City, CA) were used as an internal control. Assays were performed in triplicate with an ABI Prism 7900 sequence detector (Applied Biosystems). Data were normalized to 18S ribosomal RNA (ΔΔCt analysis). CBS activity was determined as described (18, 46). Separate reactions were carried out in the presence and absence of 1.0 mM SAM to test for allosteric induction of CBS.
Calculations.
We quantified whole-body and GIT methionine, homocysteine, and CO2 kinetics as described (26, 37, 43) (see SI Appendix).
Statistics.
Data are expressed as mean ± SEM. Differences in whole-body methionine kinetics between IV and ID infusions were analyzed by paired t test. Tissue samples were analyzed by paired t test and nonparametric Mann–Whitney test. A value of P < 0.05 was considered to be statistically significant. All statistical analyses were performed by using SPSS version 11.0 (SPSS, Chicago, IL).
Supplementary Material
Acknowledgments
We thank Liwei Cui, Xiaoyan Chang, Steve Avery, Jeremy Cottrell, and John Stephens for assistance in completing the study. This work is a publication of the USDA/ARS Children's Nutrition Research Center, Department of Pediatrics, Baylor College of Medicine and Texas Children's Hospital, Houston, TX. This work was supported by federal funds from the U.S. Department of Agriculture, Agricultural Research Service under Cooperative Agreement 58-6250-6-001 and by National Institutes of Health Grant HD33920 (to D.G.B.). M.A.R. was supported by the Sophia Research Foundation (Rotterdam, The Netherlands) and the Numico Research Foundation.
Abbreviations
- GIT
gastrointestinal tissues
- ID
intraduodenal
- IV
intravenous
- MPE
mole percent excess
- CBS
cystathionine β-synthase
- SAM
S-adenosylmethionine.
Footnotes
The authors declare no conflict of interest.
This article is a PNAS direct submission.
This article contains supporting information online at www.pnas.org/cgi/content/full/0607965104/DC1.
References
- 1.Brosnan JT, Brosnan ME. J Nutr. 2006;136:1636S–1640S. doi: 10.1093/jn/136.6.1636S. [DOI] [PubMed] [Google Scholar]
- 2.Hogeveen M, Blom HJ, Van Amerongen M, Boogmans B, Van Beynum IM, Van De BM. J Pediatr. 2002;141:429–431. doi: 10.1067/mpd.2002.126598. [DOI] [PubMed] [Google Scholar]
- 3.Hobbs CA, Cleves MA, Melnyk S, Zhao W, James SJ. Am J Clin Nutr. 2005;81:147–153. doi: 10.1093/ajcn/81.1.147. [DOI] [PubMed] [Google Scholar]
- 4.Selhub J. J Nutr. 2006;136(Suppl 6):1726S–1730S. doi: 10.1093/jn/136.6.1726S. [DOI] [PubMed] [Google Scholar]
- 5.Seshadri S, Beiser A, Selhub J, Jacques PF, Rosenberg IH, D'Agostino RB, Wilson PW, Wolf PA. N Engl J Med. 2002;346:476–483. doi: 10.1056/NEJMoa011613. [DOI] [PubMed] [Google Scholar]
- 6.Stipanuk MH. Annu Rev Nutr. 2004;24:539–577. doi: 10.1146/annurev.nutr.24.012003.132418. [DOI] [PubMed] [Google Scholar]
- 7.van der Put NM, Van Straaten HW, Trijbels FJ, Blom HJ. Exp Biol Med (Maywood) 2001;226:243–270. doi: 10.1177/153537020122600402. [DOI] [PubMed] [Google Scholar]
- 8.El Khairy L, Vollset SE, Refsum H, Ueland PM. Am J Clin Nutr. 2003;77:467–472. doi: 10.1093/ajcn/77.2.467. [DOI] [PubMed] [Google Scholar]
- 9.Akoglu B, Milovic V, Caspary WF, Faust D. Eur J Nutr. 2004;43:93–99. doi: 10.1007/s00394-004-0446-6. [DOI] [PubMed] [Google Scholar]
- 10.Danese S, Sgambato A, Papa A, Scaldaferri F, Pola R, Sans M, Lovecchio M, Gasbarrini G, Cittadini A, Gasbarrini A. Am J Gastroenterol. 2005;100:886–895. doi: 10.1111/j.1572-0241.2005.41469.x. [DOI] [PubMed] [Google Scholar]
- 11.Pufulete M, Al Ghnaniem R, Khushal A, Appleby P, Harris N, Gout S, Emery PW, Sanders TA. Gut. 2005;54:648–653. doi: 10.1136/gut.2004.054718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim YI. J Nutr. 2005;135:2703–2709. doi: 10.1093/jn/135.11.2703. [DOI] [PubMed] [Google Scholar]
- 13.Ma DW, Finnell RH, Davidson LA, Callaway ES, Spiegelstein O, Piedrahita JA, Salbaum JM, Kappen C, Weeks BR, James J, et al. Cancer Res. 2005;65:887–897. [PMC free article] [PubMed] [Google Scholar]
- 14.Gaull GE, Raiha NC, Saarikoski S, Sturman JA. Pediatr Res. 1973;7:908–913. doi: 10.1203/00006450-197311000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Shew SB, Keshen TH, Jahoor F, Jaksic T. J Pediatr Surg. 2005;40:52–56. doi: 10.1016/j.jpedsurg.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 16.Zlotkin SH, Anderson GH. Am J Clin Nutr. 1982;36:862–867. doi: 10.1093/ajcn/36.5.862. [DOI] [PubMed] [Google Scholar]
- 17.Pohlandt F. Acta Paediatr Scand. 1974;63:801–804. doi: 10.1111/j.1651-2227.1974.tb04866.x. [DOI] [PubMed] [Google Scholar]
- 18.Mudd SH, Finkelstein JD, Irreverre F, Laster L. J Biol Chem. 1965;240:4382–4392. [PubMed] [Google Scholar]
- 19.Stegink LD, Den Besten L. Science. 1972;178:514–516. doi: 10.1126/science.178.4060.514. [DOI] [PubMed] [Google Scholar]
- 20.Hiramatsu T, Fukagawa NK, Marchini JS, Cortiella J, Yu YM, Chapman TE, Young VR. Am J Clin Nutr. 1994;60:525–533. doi: 10.1093/ajcn/60.4.525. [DOI] [PubMed] [Google Scholar]
- 21.Raguso CA, Ajami AM, Gleason R, Young VR. Am J Clin Nutr. 1997;66:283–292. doi: 10.1093/ajcn/66.2.283. [DOI] [PubMed] [Google Scholar]
- 22.Shoveller AK, Brunton JA, House JD, Pencharz PB, Ball RO. J Nutr. 2003;133:4215–4224. doi: 10.1093/jn/133.12.4215. [DOI] [PubMed] [Google Scholar]
- 23.Shoveller AK, House JD, Brunton JA, Pencharz PB, Ball RO. J Nutr. 2004;134:609–612. doi: 10.1093/jn/134.3.609. [DOI] [PubMed] [Google Scholar]
- 24.Bos C, Stoll B, Fouillet H, Gaudichon C, Guan X, Grusak MA, Reeds PJ, Tome D, Burrin DG. Am J Physiol. 2003;285:E1246–E1257. doi: 10.1152/ajpendo.00150.2003. [DOI] [PubMed] [Google Scholar]
- 25.Stoll B, Henry J, Reeds PJ, Yu H, Jahoor F, Burrin DG. J Nutr. 1998;128:606–614. doi: 10.1093/jn/128.3.606. [DOI] [PubMed] [Google Scholar]
- 26.van Goudoever JB, Stoll B, Henry JF, Burrin DG, Reeds PJ. Proc Natl Acad Sci USA. 2000;97:11620–11625. doi: 10.1073/pnas.200371497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lobley GE, Shen X, Le G, Bremner DM, Milne E, Calder AG, Anderson SE, Dennison N. Br J Nutr. 2003;89:617–630. doi: 10.1079/BJN2003831. [DOI] [PubMed] [Google Scholar]
- 28.Prudova A, Bauman Z, Braun A, Vitvitsky V, Lu SC, Banerjee R. Proc Natl Acad Sci USA. 2006;103:6489–6494. doi: 10.1073/pnas.0509531103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bos C, Stoll B, Fouillet H, Gaudichon C, Guan X, Grusak MA, Reeds PJ, Burrin DG, Tome D. Am J Physiol. 2005;288:E436–E446. doi: 10.1152/ajpendo.00263.2004. [DOI] [PubMed] [Google Scholar]
- 30.Stoll B, Burrin DG, Henry JF, Jahoor F, Reeds PJ. Am J Physiol. 1999;276:G49–G57. doi: 10.1152/ajpgi.1999.276.1.G49. [DOI] [PubMed] [Google Scholar]
- 31.Shoveller AK, Brunton JA, Pencharz PB, Ball RO. J Nutr. 2003;133:1390–1397. doi: 10.1093/jn/133.5.1390. [DOI] [PubMed] [Google Scholar]
- 32.Finkelstein JD. Semin Thromb Hemost. 2000;26:219–225. doi: 10.1055/s-2000-8466. [DOI] [PubMed] [Google Scholar]
- 33.Townsend JH, Davis SR, Mackey AD, Gregory JF., III Am J Physiol. 2004;286:G588–G595. doi: 10.1152/ajpgi.00454.2003. [DOI] [PubMed] [Google Scholar]
- 34.Malmezat T, Breuille D, Pouyet C, Buffiere C, Denis P, Mirand PP, Obled C. Am J Physiol Endocrinol Metab. 2000;279:E1391–E1397. doi: 10.1152/ajpendo.2000.279.6.E1391. [DOI] [PubMed] [Google Scholar]
- 35.Vitvitsky V, Mosharov E, Tritt M, Ataullakhanov F, Banerjee R. Redox Rep. 2003;8:57–63. doi: 10.1179/135100003125001260. [DOI] [PubMed] [Google Scholar]
- 36.Lobley GE, Connell A, Revell D. Br J Nutr. 1996;75:47–56. doi: 10.1079/bjn19960109. [DOI] [PubMed] [Google Scholar]
- 37.MacCoss MJ, Fukagawa NK, Matthews DE. Am J Physiol. 2001;280:E947–E955. doi: 10.1152/ajpendo.2001.280.6.E947. [DOI] [PubMed] [Google Scholar]
- 38.Tessari P, Kiwanuka E, Coracina A, Zaramella M, Vettore M, Valerio A, Garibotto G. Am J Physiol. 2005;288:E1270–E1276. doi: 10.1152/ajpendo.00383.2004. [DOI] [PubMed] [Google Scholar]
- 39.Stead LM, Brosnan JT, Brosnan ME, Vance DE, Jacobs RL. Am J Clin Nutr. 2006;83:5–10. doi: 10.1093/ajcn/83.1.5. [DOI] [PubMed] [Google Scholar]
- 40.Van Klinken BJ, Einerhand AW, Buller HA, Dekker J. Anal Biochem. 1998;265:103–116. doi: 10.1006/abio.1998.2896. [DOI] [PubMed] [Google Scholar]
- 41.Stoll B, Burrin DG, Henry J, Yu H, Jahoor F, Reeds PJ. Am J Physiol. 1999;277:E168–E175. doi: 10.1152/ajpendo.1999.277.1.E168. [DOI] [PubMed] [Google Scholar]
- 42.Davis SR, Stacpoole PW, Williamson J, Kick LS, Quinlivan EP, Coats BS, Shane B, Bailey LB, Gregory JF., III Am J Physiol. 2004;286:E272–E279. doi: 10.1152/ajpendo.00351.2003. [DOI] [PubMed] [Google Scholar]
- 43.Storch KJ, Wagner DA, Burke JF, Young VR. Am J Physiol. 1988;255:E322–E331. doi: 10.1152/ajpendo.1988.255.3.E322. [DOI] [PubMed] [Google Scholar]
- 46.Lambert BD, Titgemeyer EC, Stokka GL, DeBey BM, Loest CA. J Nutr. 2002;132:2004–2009. doi: 10.1093/jn/132.7.2004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.