Abstract
To investigate whether therapy with alpha interferon (IFN-α) induces changes in intrahepatic antigen-presenting cells (APCs), we obtained liver biopsy specimens before, during, and after therapy with IFN-α from chronic hepatitis B patients whose viral load had already been reduced by at least 8 weeks of treatment with lamivudine. HLA-DR, CD1a, and CD83 were not modified by the therapy. The intralobular expression of CD68 on Kupffer cells remained stable, denoting no changes in the number of resident macrophages during IFN-α treatment. In contrast, CD14 was weakly expressed in the absence of IFN-α and was significantly up-regulated during therapy. At the same time, the levels of soluble CD14 and interleukin-10 in plasma increased significantly. In vitro, monocytes maintained in the presence of IFN-α differentiated into macrophages or dendritic cells with higher levels of expression of CD14 than that for the control cultures. During therapy with IFN-α, T-cell infiltration in the portal spaces was reduced, mainly due to a significant decrease in the number of CD8+ T cells. These findings show that IFN-α is biologically active on APCs in vivo and in vitro and suggest that this newly described regulatory function, together with the already known inhibitory effects on lymphocytes, may cooperate to reduce inflammation and consequent tissue damage in patients with chronic viral hepatitis.
In vitro and clinical studies have repeatedly shown how alpha interferon (IFN-α) is essential in initiating the cascades of events leading to effective antiviral immune responses and to the containment of viral replication (7, 18). Since their discovery, type I IFNs have been known to exert direct antiviral activity through the induction of cellular proteins that interfere with virus replication (9). However, evidence is accumulating that viruses have developed a variety of escape mechanisms, such as the production of proteins that mimic IFN receptors or that interfere with the signal pathways of apoptosis and that therefore hamper the first crucial antiviral defense (7, 41).
Type I IFNs also display a wide array of effects on immune responses, such as the enhancement of T- and NK-cell cytotoxic activities and the inhibition of suppressor activity, as well as the inhibition of in vitro lymphocyte proliferation through interference with interleukin-2 (IL-2)-induced signals (4, 13). A crucial role of type I IFNs in linking innate and adaptive immunity was already suggested by early work showing that IFN-α is able to drive the differentiation of CD14+ monocytes into dendritic cells (DCs) both in vitro and in vivo (15, 31), therefore providing the necessary conditions for the priming of naïve T lymphocytes. Moreover, direct stimulation of natural IFN-producing cells by infectious and noninfectious viral particles stimulates such cells to produce large amounts of type I IFNs and triggers differentiation into DCs (19, 38).
Inadequate antiviral immune responses are thought to be the foundation for the establishment of virus persistence in patients with chronic hepatitis B and C, conditions in which the clinical use of IFN-α has proved beneficial and has resulted in sustained viral clearance in at least a proportion of patients (34). It is believed that the immunomodulatory properties of IFN-α play an important role in the resolution of persistent infection (6). The liver represents a unique environment with respect to cells with antigen (Ag)-presenting function. Liver sinusoid endothelial cells, which separate and protect hepatocytes from blood-borne leukocytes, have been shown to induce Ag-specific tolerance in CD8+ T lymphocytes (29). Kupffer cells, the resident liver macrophages patrolling the sinusoids, and intrahepatic DCs have been demonstrated to produce IL-10, which down-regulates both Ag presentation and T-cell activation (16, 23). It has been proposed that the physiological liver milieu also affects the maturation of DCs and may therefore generate a tolerogenic DC phenotype (49). These features of liver Ag-presenting cells (APCs) could be responsible at least in part for the weak antiviral responses that allow the persistence of hepatitis viruses. We therefore hypothesized that treatment with IFN-α may contribute to the generation of antiviral responses through the modification of intrahepatic APCs. To test this hypothesis, we investigated whether IFN-α administration to chronic hepatitis B (CHB) patients induces changes in the numbers and/or the phenotypes of liver APCs that could result in potent T-cell stimulation and evaluated the degree of lymphocytic infiltration.
We conducted an immunohistochemical study with samples from patients who received IFN-α after a short treatment with lamivudine, a nucleoside analogue that has recently been introduced as therapy for CHB and that is known to achieve significant reductions in the hepatitis B virus (HBV) load (27). This choice was urged by the need to abolish or minimize possible confounding factors, most of all the amelioration or amplification of the antiviral immune response consequent to a marked reduction of the viral load (3) and, thus, to separate this event from the immunotherapeutic characteristics of IFN-α. In the present study, we show that IFN-α, given to CHB patients whose viral loads and disease activities were already minimized by lamivudine administration, does not detectably modify the distribution of DCs or macrophages within the liver. However, it significantly increases the level of expression of CD14 on liver macrophages and contributes to a reduction in the level of infiltrating CD8+ T lymphocytes while increasing the levels of soluble CD14 (sCD14) and IL-10 in plasma.
MATERIALS AND METHODS
Samples.
Liver biopsy and blood samples were obtained from 11 patients with chronic HBV infection who were negative for markers of human immunodeficiency virus, hepatitis C virus, and hepatitis D virus infections. These patients, who had been already receiving lamivudine (150 mg/day) for periods ranging from 15 to 41 weeks (median, 17.5 weeks), were treated with a combination of lamivudine and IFN-α for 8 weeks (14 weeks in one patient) and then with IFN-α alone for a further 8 weeks (18 weeks in two patients). IFN-α2b (Intron A; Schering-Plough, Kenilworth, N.J.) was administered subcutaneously at a dose of 10 MU/day for 4 weeks and then at a dose of 10 MU three times/week. Liver biopsy specimens were obtained by needle percutaneous puncture (i) immediately before IFN-α administration was started (time zero [t0]); (ii) early during combined lamivudine-IFN-α therapy (t1), between 18 and 39 days (median, 27 weeks) after IFN-α was started; and (iii) 14 to 20 weeks (median, 16 weeks) after therapy was interrupted (t2). The alanine aminotransferase (ALT) levels and the HBV DNA loads measured in sera collected concomitantly with the liver biopsy specimens, as well as in retrospective samples obtained prior to lamivudine monotherapy, are reported in Table 1. HBV DNA was quantified by the Hybrid Capture Assay II (detection limit, 1.4 × 105 genome equivalents [geq]/ml; Digene, Gaithersburg, Md.) and, if the result was negative, by quantitative PCR (Amplicor HBV Monitor test; detection limit, 1 × 103 geq/ml; Roche Diagnostics Corporation, Indianapolis, Ind.), followed by qualitative PCR (detection limit, 400 geq/ml) (35). Informed consent was obtained from all patients for the recovery of the three sequential liver biopsy specimens and the additional blood samples. The subjects were part of a larger group of patients who underwent a pilot trial and who were treated with lamivudine and IFN-α combined. The trial was approved by the local ethical committee, in conformity with the ethical guidelines of the 1975 Declaration of Helsinki.
TABLE 1.
ALT levels and HBV DNA loads in the patients included in the study prior to lamivudine therapy and at different times of liver biopsy specimen collectiona
| Patient no. | ALT concn (IU/liter)
|
HBV DNA load (geq/ml)
|
||||||
|---|---|---|---|---|---|---|---|---|
| t −1 | t0 | t1 | t2 | t −1 | t0 | t1 | t2 | |
| 1 | 362 | 30 | 122 | 31 | 1.3 × 109 | 1.0 × 103 | 1.1 × 103 | 1.0 × 103 |
| 2 | 31 | 60 | 44 | 26 | 3.0 × 109 | 2.4 × 105 | 2.8 × 104 | 1.7 × 109 |
| 3 | 96 | 17 | 23 | 45 | 9.3 × 108 | 1.5 × 105 | 9.5 × 103 | 6.2 × 109 |
| 4 | 80 | 30 | 119 | 232 | 1.2 × 109 | 5.9 × 106 | 2.7 × 104 | 1.1 × 109 |
| 5 | 28 | 22 | 25 | 33 | NDb | 4 × 102 | 4 × 102 | 2.1 × 105 |
| 6 | 79 | 41 | 29 | 26 | 2.8 × 1010 | 6.8 × 107 | 9.4 × 106 | 1.5 × 109 |
| 7 | 28 | 51 | 172 | 78 | 4.0 × 108 | 3.9 × 104 | 2.4 × 103 | 6.6 × 108 |
| 8 | 21 | 12 | 98 | 35 | 6.0 × 108 | 3.1 × 105 | 2.1 × 104 | 9.2 × 108 |
| 9 | 190 | 61 | 76 | 17 | 2.1 × 109 | 4.0 × 102 | 1.0 × 103 | 4.0 × 102 |
| 10 | 70 | 50 | 98 | 727 | 5.8 × 107 | 1.9 × 105 | 4.0 × 102 | 2.1 × 108 |
| 11 | 35 | 38 | 87 | 52 | 5.7 × 108 | 2.3 × 105 | 7.6 × 103 | 1.2 × 109 |
The upper limits of normal ALT levels are 31 IU/liter in females and 41 IU/liter in males. t −1, no treatment (i.e., prior to the start of lamivudine treatment). t0 to t2 are defined in the text.
ND, not done.
Immunohistochemistry.
Immunohistochemical staining was performed with sections of liver tissue. Two fragments from each specimen were fixed in formalin and snap-frozen in liquid nitrogen, respectively. Sections of formalin-fixed tissue were used for immunostaining of T-cell markers CD3, CD4, and CD8, whereas cryostat sections were stained for APC markers CD68, CD14, CD1a, CD83, and HLA-DR. Paraffin-embedded formalin-fixed tissue sections (4 μm) mounted on coated slides (Klinipath, Duiven, The Netherlands) were deparaffinized, rehydrated, and boiled for 15 min in citric acid buffer (10 mM; pH 6.0) by using a microwave oven. The slides were washed with phosphate-buffered saline (PBS)-0.05% Tween 20 (Fluka Chemie AG, Buchs, Switzerland) and incubated with primary antibody (Ab; CD3 or CD8 [DAKO, Glostrup, Denmark] or CD4 [Novocastra, Newcastle upon Tyne, United Kingdom]) for 1 h. After the sections were washed, they were incubated with the appropriate labeled secondary Ab (SwαR-horseradish peroxidase [HRP] or RαM-HRP [DAKO] or biotinylated Gα polyvalent [Lab Vision Corporation, Fremont, Calif.]) for 1 h at room temperature. After a washing step, the slides were incubated with a tertiary reagent (RαSw-HRP or SwαR-HRP [DAKO] or streptavidin-HRP [Lab Vision]) for 1 h at room temperature. HRP activity was revealed by incubating the slides in 3-amino-9-ethylcarbazole (Sigma Chemical Co., St. Louis, Mo.) solution for 10 min, which resulted in a bright red precipitate. Markers of HBV infection, namely, HBsAg and HBcAg, were also detected on paraffin sections by a similar immunohistochemical technique. Primary Abs were polyclonal rabbit anti-HBc (DAKO) and monoclonal mouse anti-HBs (BioGenex, San Ramon, Calif.). An UltraVision detection system (Lab Vision) was used to visualize positive cells, according to the instructions of the manufacturer.
Cryostat sections (6 μm), mounted on 0.1% gelatin- and 0.01% chromium potassium sulfate-coated slides, were fixed in acetone (purity, >99.5%; Fluka) supplemented with 0.5% H2O2 for 10 min at room temperature. Endogenous peroxidase was revealed as material that stained dark blue with 4-chloro-1-naphthol (Sigma). The slides were washed with PBS-0.05% Tween 20 and incubated with primary Ab (HLA-DR [L243; Coulter Clone, Hialeah, Fla.], CD68 [KP-1; DAKO], CD14 [MY-14; Coulter Clone], CD1a [OKT-6; DAKO], or CD83 [M43; Immunotech, Westbrook, Maine]) overnight at 4°C. A secondary Ab (RαM-HRP; DAKO) and a tertiary Ab (SwαR-HRP; DAKO) were incubated, and peroxidase activity was revealed as described above for the paraffinized sections. For both the paraffinized and the cryostat sections, counterstaining with hematoxylin was performed after the 3-amino-9-ethylcarbazole color development reaction. For both the cryostat and the paraffinized sections, a human tonsil tissue specimen was included in each staining reaction as an internal positive control. Omission of the primary Ab was included as a negative control in each staining reaction.
The T cells in portal space infiltrates were analyzed by microscope examination and assessment of a score from 0 to 3, as follows: 0, no positive cells; 1, ≤25% positive cells; 2, >25% and ≤50% positive cells; and 3, >50% positive cells. On average, six portal spaces (minimum, 3 portal spaces; maximum, 13 portal spaces) were analyzed in each section. The portal spaces and liver parenchyma were qualitatively analyzed for APC markers, with the exception of CD14+ cells, which were enumerated by averaging the number of positive cells in three to five microscope fields (magnification, ×400; area per microscope field, 0.175 mm2) and expressed as the number of positive cells per high-power field (hpf). Two independent observers carried out all microscopy evaluations; they were unaware of the specificity of the staining, the sampling time, and the patient from whom the material was obtained.
Serum cytokines and sCD14.
Serum samples were tested for the levels of circulating IL-10 and IL-12 p70 by a standard sandwich enzyme-linked immunosorbent assay (ELISA) technique. Abs for coating and detection and ELISA reagents were obtained from BD Biosciences/Pharmingen (San Diego, Calif.) (anti-IL-10) and R&D Systems (Minneapolis, Minn.) (anti-IL-12). The lower detection limits were 4 and 16 pg/ml for IL-10 and IL-12, respectively. sCD14 levels in serum were measured with a commercial ELISA kit (Quantikine human sCD14 immunoassay; R&D Systems). According to the manufacturer, normal serum sCD14 levels range from 0.8 to 3.2 μg/ml (average, 1.9 μg/ml).
Culture and phenotype of monocyte-derived cells.
Freshly isolated peripheral blood mononuclear cells from healthy donors were incubated in RPMI 1640 medium containing 2% pooled human serum for 2 h at 37°C in 25-cm2 tissue culture flasks (Costar, Cambridge, Mass.). Nonadherent cells were discarded, and after extensive washing with serum-free RPMI 1640 medium, adherent cells were cultured in RPMI 1640 medium containing 20% human serum. This culture protocol consistently yields preparations containing >98% macrophages. Clinical grade IFN-α (Intron A; Schering-Plough) was added to selected cultures at 1,000 IU/ml either at the beginning of the culture period or 1 week after the beginning of culture, that is, after the maturation of monocytes into macrophages had occurred. To prepare cell suspensions, monocyte-derived macrophages were rinsed extensively with PBS, incubated with PBS containing 0.5 mM EDTA at 37°C for 15 min, and then detached by gentle scraping. Monocyte-derived DCs were prepared essentially as described by Romani et al. (39). Adherent cells, prepared as described above for macrophage generation, were cultured in RPMI 1640 medium containing 10% fetal calf serum, 50 ng of granulocyte-macrophage colony-stimulating factor (GM-CSF; R&D Systems) per ml, and 50 ng of IL-4 (R&D Systems) per ml at 37°C for 6 days. At the end of the culture period, 60 to 85% of the cells were nonadherent and displayed a phenotype typical of that of immature DCs (CD14−, CD1a+, CD83−). Detached macrophages and DCs were resuspended in PBS containing 0.2% sodium azide and 2% fetal calf serum, and the suspension was incubated with phycoerythrin-conjugated CD14 Ab (clone M5E2; BD Biosciences/Pharmingen), phycoerythrin-conjugated CD86 Ab (clone HA5.2B7; Immunotech, Marseille, France), fluorescein isothiocyanate-conjugated CD80 Ab (clone MAB104; Immunotech), or an isotype control for 20 min on ice and then washed and resuspended in 1% paraformaldehyde in PBS. The cells were analyzed in a FACScan flow cytometer (BD Biosciences) with CellQuest software.
Statistical analysis.
Comparison of paired data for the patients at different times of follow-up was performed by Wilcoxon's signed-rank test.
RESULTS
IFN-α up-regulates CD14 expression on intrahepatic macrophages.
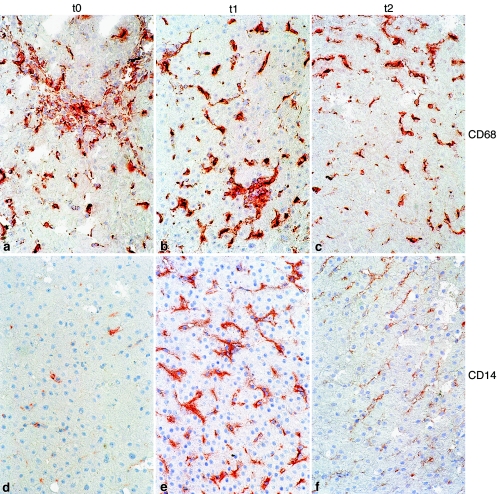
To investigate whether IFN-α administration results in changes to the intrahepatic APC pool, we analyzed the expression of HLA-DR and CD68, common to macrophages and DCs, of the monocyte/macrophage marker CD14 and the expression of CD1a and CD83, which are expressed on immature, skin-associated DCs and mature DCs, respectively. No staining for CD1a was observed at any time point. CD83 was clearly detected in control tonsil tissue but was detected only in four liver biopsy specimens from three patients, which stained weakly, suggesting that mature DCs were not present in significant amounts in the livers of the patients studied (data not shown). Large numbers of intraparenchymal CD68+ cells were seen. No significant changes in the number of CD68+ cells or the staining intensity were observed at the three time points studied (Fig. 1a to c). Staining for HLA-DR resulted in a pattern similar to that of staining for CD68 (data not shown).
FIG. 1.
Phenotypes of liver macrophages determined by immunohistochemical staining of CD68+ (a to c) and CD14+ (d to f) cells in representative liver biopsy specimens during lamivudine monotherapy at time of IFN-α addition (t0) (a and d), early during combined lamivudine and IFN-α administration (t1) (b and e), and in the absence of therapy (t2) (c and f). Magnifications, ×400.
An increase in the numbers of CD14+ cells was detected at t1 in comparison with the numbers detected at t0. The expression of CD14 was weak and was limited to a small number of cells in liver biopsy specimens at t0 (Fig. 1d). IFN-α administration was associated with increased staining intensity and increased numbers of CD14+ intralobular cells in the biopsy specimens at t1 (Fig. 1e), but these were no longer detectable after therapy was withdrawn (Fig. 1f). Figure 2 shows the variations in the numbers of CD14+ cells/hpf in individual patients. Increased numbers of CD14+ cells were seen at t1 (Fig. 2, left panel) in 10 of the 11 patients studied in comparison to the numbers detected at t0 (1.1 to 11 times the number of positive cells at t0; P = 0.008). The six patients from whom frozen material from the third biopsy was available showed numbers of CD14+ cells/hpf at t2 not significantly different from those observed at t0 (data not shown).
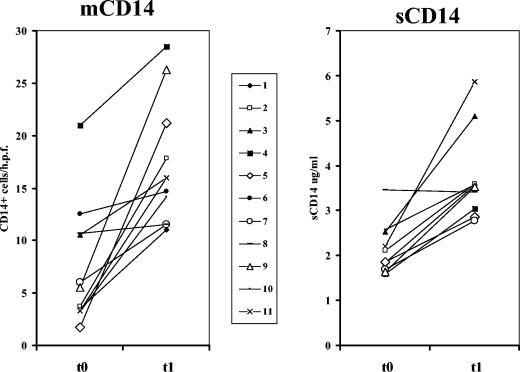
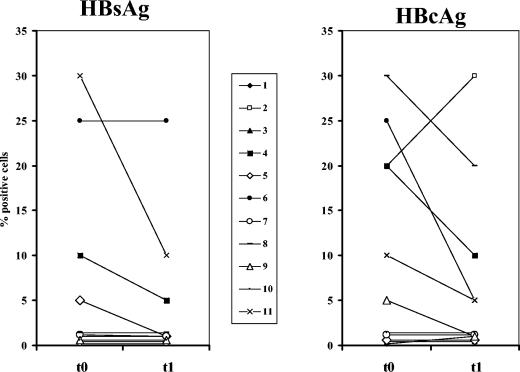
FIG. 2.
(Left panel) IFN-α increases CD14 expression in liver tissue. The average numbers of CD14+ liver macrophages (mCD14) per hpf (0.175 mm2) for individual biopsy specimens taken at t0 and t1, before and after the addition of IFN-α to lamivudine, respectively, are shown. (Right panel) sCD14 levels measured in sera collected at t0 and t1. The levels of sCD14 were higher at t1 and were above the normal levels in seven samples (normal range, 0.8 to 3.2 μg/ml).
Circulating sCD14 and IL-10 levels increase during IFN-α treatment.
The increased levels of CD14 expression on liver macrophages led us to investigate whether the administration of IFN-α was also inducing systemic changes that could be related to modification of APC secretion patterns and/or activation. As shown in Fig. 2 (right panel), serum sCD14 levels before IFN-α administration (t0) were distributed within the normal range of values (mean ± standard deviation [SD] = 2.06 ± 0.61 μg/ml). During IFN-α therapy (t1), all except one of the patients showed increased sCD14 levels, and in seven of the patients the levels exceeded the normal range (mean ± SD = 3.62 ± 1.00 μg/ml; P < 0.001 versus the levels at t0). It is interesting that the only patient whose sCD14 levels were not modified by IFN-α administration also did not show modifications in the number of CD14+ cells in liver tissue (Fig. 2, left panel).
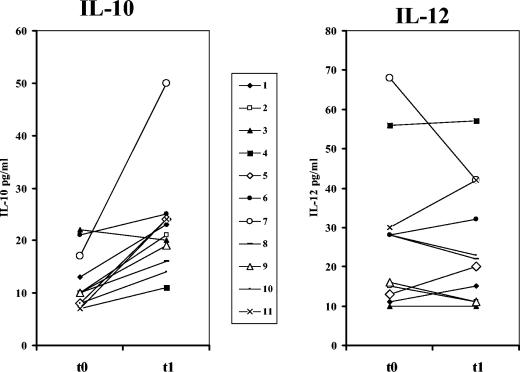
We also measured the levels of IL-10 and IL-12 in the circulation. Serum samples collected on the same day on which the first two liver tissue specimens were obtained, before IFN-α administration and early during dual therapy, showed statistically significant increases in IL-10 levels (P = 0.011), whereas IL-12 levels remained unchanged (Fig. 3).
FIG. 3.
Circulating cytokines during IFN-α therapy. Serum IL-10 and IL-12 levels during lamivudine monotherapy at the time of IFN-α addition (t0) and early during combined therapy with lamivudine and IFN-α (t1) are shown.
Reduced CD8+ T-cell intrahepatic infiltration.
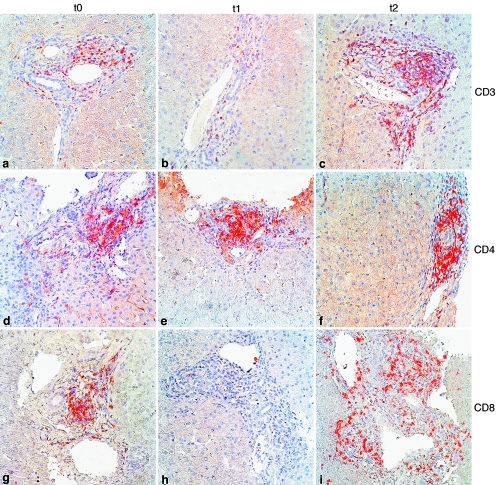
In all patients we found mild to moderate mononuclear cell infiltrates in the portal spaces at all time points, with no evidence of aggressive disease, as indicated by the absence of a translobular infiltrate and interphase hepatitis. At t0, the average ± SD score for CD3+ cells was 2.3 ± 0.6, indicating a predominant (>50%) T-cell population among the infiltrating cells. CD4 and CD8 subsets were equally represented, with scores of 1.4 ± 0.7 and 1.3 ± 0.5, respectively. A decrease in the relative amount of infiltrating T cells was observed early during IFN-α treatment (t1). The CD3+ cell score was 1.5 ± 0.5, which was significantly lower than that found at t0 (P = 0.02). A reduction in the fraction of infiltrating CD3+ cells was paralleled by a decrease in the relative amount of infiltrating CD8+ T cells, whose average score was 0.9 ± 0.3. The relative amount of CD4+ T cells did not differ between t0 and t1, with the score at t1 being 1.3 ± 0.7. Analysis of the specimens obtained after therapy was interrupted (t2) yielded a picture comparable to that seen at t0, with scores of 2.2 ± 0.6, 1.4 ± 0.9, and 1.3 ± 0.4 for CD3+, CD4+, and CD8+ infiltrating cells, respectively. Figure 4 shows the distribution of CD3+, CD4+, and CD8+ cells in a patient whose scores closely matched the average ones.
FIG. 4.
Phenotypes of infiltrating T cells in liver biopsy specimens determined by immunohistochemical staining of CD3+ (a to c), CD4+ (d to f), and CD8+ (g to i) T lymphocytes in representative portal spaces during lamivudine monotherapy at the time of IFN-α addition (t0) (a, d, and g), early during combined lamivudine and IFN-α administration (t1) (b, e, and h), and in the absence of therapy (t2) (c, f, and i). Magnifications, ×400.
Amounts of infected cells decrease during IFN-α therapy.
Immunohistochemical detection of HBsAg and HBcAg revealed the presence of HBV-infected hepatocytes in a fraction of the patients studied. Before IFN-α treatment was started, nuclear HBcAg was detected in 5 to 30% of the hepatocytes in 6 of the 11 patients, with the other patients showing no or sporadic positive cells. A similar picture was revealed with anti-HBs Abs, which showed the presence of the HBV surface Ag in 5 to 30% of the hepatocytes in four patients. At t1, after the addition of IFN-α treatment, these percentages were reduced in three of four patients for HBsAg (Fig. 5, left panel) and in five of six patients for HBcAg (Fig. 5, right panel). However, this reduction was not statistically significant, given the high number of patients with sporadic or no positive staining for viral Ags at both time points.
FIG. 5.
Percentage of hepatocytes that scored positive for HBsAg (left panel) or HBcAg (right panel) before and after the addition of IFN-α to lamivudine treatment.
IFN-α counteracts the down-regulation of CD14 on DCs and macrophages in vitro.
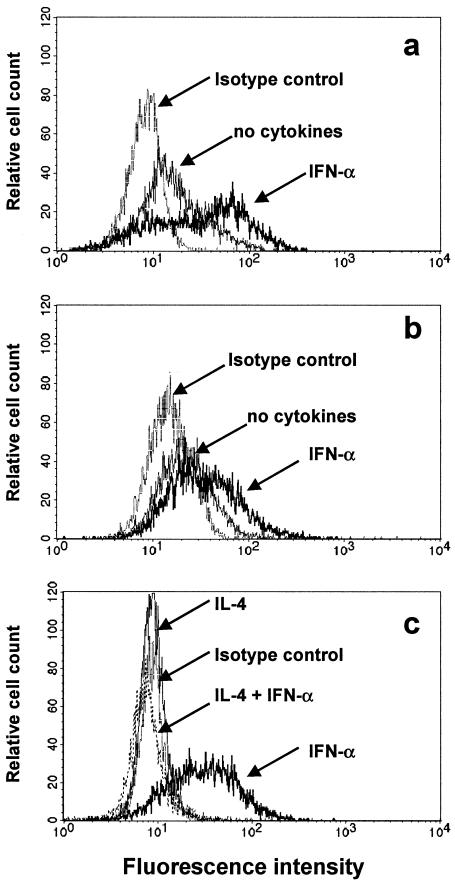
To test whether IFN-α can directly affect CD14 expression on APCs, we subjected human peripheral blood monocytes from three healthy donors to in vitro culture in IFN-α-containing medium. CD14 expression on peripheral blood monocytes was not modified by a 6-h incubation in IFN-α-containing medium. Standard 6- or 12-day culture of peripheral blood monocytes in the presence of human serum resulted in the down-regulation of CD14 and the acquisition of the typical morphology and phenotype of macrophages. As shown in Fig. 6a, IFN-α counteracted the physiological down-regulation of CD14 when it was added at the beginning of the culture, yielding macrophages that expressed CD14 at levels higher than those of macrophages cultured in the absence of the cytokine. Similarly, the addition of IFN-α after 6 days of culture prevented further down-regulation of CD14 in the subsequent 6-day period (Fig. 6b). No differences in morphology were observed when macrophages cultured in the presence or the absence of IFN-α were compared, and the effect of IFN-α was consistently detected in our experiments. The expression of the costimulatory molecule CD86 was not affected either by the culture procedure or by the addition of IFN-α. CD80 was not significantly expressed by fresh or cultured monocytes/macrophages under any of the conditions tested in this set of experiments (data not shown).
FIG. 6.
In vitro phenotypes of monocyte-derived macrophages and DCs cultured in the presence or the absence of IFN-α. Higher levels of CD14 expression were detected in the presence of IFN-α, added either at the beginning of culture (a) or after maturation to macrophages occurred (b). DCs obtained in the presence of GM-CSF, IL-4, and IFN-α became CD14 negative, while DCs obtained in the presence of GM-CSF and IFN-α still expressed CD14 at levels comparable to those expressed by macrophages (c).
Similar experiments were performed to assess whether IFN-α also counteracts the down-regulation of CD14, characteristic of the maturation of monocytes to DCs. When GM-CSF was used in combination with IL-4, which blocks the differentiation to macrophages and induces differentiation to immature DCs (40), CD14 was completely down-regulated within 5 days. At the beginning of culture the addition of IFN-α to the combination GM-CSF and IL-4 did not affect the down-regulation of CD14 (Fig. 6c), nor did IFN-α modify CD14 expression when it was added later, e.g., after differentiation to immature DCs had already occurred (data not shown). However, culture of monocytes for 5 days in the presence of GM-CSF and IFN-α instead of GM-CSF and IL-4, a protocol known to induce rapid maturation to potent Th1-inducing DCs (43), yielded cells that still expressed CD14 (Fig. 6c). These DCs had acquired a morphology indistinguishable from that of cells treated with GM-CSF and IL-4. All DCs strongly expressed CD86, regardless of the combination of cytokines used. CD80, which was present at low levels on cells treated with GM-CSF and IL-4 or which was absent from cells treated with GM-CSF and IL-4, was up-regulated by the combination IFN-α and GM-CSF, regardless of the presence of IL-4. Moreover, DCs treated with GM-CSF and IFN-α expressed CD83 (data not shown).
DISCUSSION
We provide here evidence that a qualitative rather than a quantitative change in the intrahepatic pool of professional APCs occurs in CHB patients undergoing IFN-α therapy. This is reflected mainly in the increased level of expression of the surface marker CD14 on Kupffer cells, but expression returns to the baseline level after the discontinuation of therapy. At the systemic level, the plasma sCD14 concentration increased above the normal range of concentrations during IFN-α administration. CD14, a 55-kDa glycoprotein expressed on myeloid cells, is the major receptor for bacterial lipopolysaccharide (LPS) (14) and peptidoglycan (11) and also interacts with some viral proteins (26). CD14 is an essential component of the LPS receptor complex that includes an LPS-binding protein, the myeloid differentiation protein-2 (MD-2), and the transmembrane signaling Toll-like receptor-4 (TLR-4) (14). Experiments with rodents suggest that proinflammatory cytokines such as IL-1β and tumor necrosis factor alpha are involved in the LPS-induced expression of CD14 on Kupffer cells (30, 33). The up-regulation of CD14 on human liver macrophages has been reported during both acute and chronic active hepatitis (50), probably as the result of proinflammatory cytokine secretion, as in the LPS-induced model in rodents. In the same report (50), the level of CD14 expression in liver tissue from patients with chronic persistent hepatitis or cirrhosis was low, reflecting the absence of active liver disease. Similarly, in the patients reported on here, CD14 was minimally expressed on liver macrophages prior to IFN-α administration as well as 4 months after treatment was terminated. At both time points, disease activity was minimal, and the level of CD14 expression matched that reported in healthy livers (50). In our study, enhanced CD14 expression in the early phase of IFN-α therapy is unlikely the consequence of inflammation, as suggested by the low ALT levels and the concomitant reduction in the number of T cells infiltrating the portal space.
It has been demonstrated that in patients with CHB only a small proportion of the liver-infiltrating cytotoxic lymphocytes are virus specific. Moreover, it has been proposed that the recruitment of bystander T lymphocytes to the liver likely results from a protracted and ineffective virus-specific response and may represent a relevant cause of liver damage (5, 32). We detected few differences in the degrees and compositions of the lymphocytic infiltrates in the portal spaces during lamivudine monotherapy (more specifically, in the presence of a relatively low viral load) and at 4 months after therapy interruption, when the levels of viremia in most patients were again high. This finding suggests that the level of viral replication may have little influence per se on the recruitment of bystander cells and cells potentially damaging to the liver.
In contrast, the administration of IFN-α induced a significant reduction of liver-infiltrating immune cells due to the almost complete disappearance of CD8+ lymphocytes. This suggests that a second important effect of IFN-α seen in this group of CHB patients is its ability to halt the recruitment of bystander lymphocytes within the inflammation sites. This process has recently been shown (46) to be dependent on the release of matrix-degrading metalloproteinases, the activation of which can be inhibited by all kinds of IFNs (42).
Although disease activity and viral replication were maximally reduced during IFN-α and lamivudine combination therapy, we cannot exclude the possibility that other factors may have participated in the modulation of CD14 expression. The results of the in vitro experiments reported here provide additional evidence that IFN-α modulates the expression of CD14. Under the test conditions used, IFN-α counteracted the physiologic CD14 down-regulation that occurred during monocyte differentiation into macrophages and allowed the generation of CD14+ DCs when GM-CSF and IFN-α were used without the addition of IL-4.
It has recently been shown (10) that CD14 serves as a receptor for apoptotic cells. In contrast to the uptake of apoptotic cells by DCs, which results in the processing and presentation of Ag to T cells (1), the CD14-mediated uptake of apoptotic cells by macrophages diverts the phagocytosed antigenic material from T-cell recognition (17). This mechanism could be enhanced by the known effect of IFN-α on the CD95-mediated pathway of apoptosis: increased levels of expression of CD95 on infected cells (12, 28, 45) and the concomitant up-regulation of the Fas ligand on NK effector cells (20) may result in the accelerated apoptosis of infected cells, which in turn are removed by CD14-expressing Kupffer cells without further activation of the infiltrating lymphocytes. In line with this interpretation, we found no evidence of a significant involvement of DCs in the liver. We detected only minimal CD83 expression, a marker of mature DCs (51), in the liver specimens of CHB patients. It has recently been reported that only a small fraction of CD11c+ DCs found in the portal spaces of the livers of patients with chronic hepatitis express CD83, predominantly in sites of piecemeal necrosis (25). Our data are consistent with this finding, given the lack of active hepatitis in this group of lamivudine-treated patients, and suggest that IFN-α administration does not result in a detectable mobilization and/or maturation of intrahepatic DCs, although we cannot exclude the possibility that if the maturation of DCs has occurred, these cells may have been rapidly routed to the regional lymph nodes (24). The unchanged levels of circulating IL-12 also confirmed the lack of a significant systemic activation of DCs.
As expected, the effect of IFN-α administration was not limited to the liver. Circulating sCD14 levels were also increased at the same time that increased levels of CD14 expression on Kupffer cells were detected. sCD14 is regarded as a product of macrophage activation and appears to be involved in the down-modulation of the response to LPS during sepsis (21). Increased levels of circulating sCD14 have been reported in patients with various inflammatory states, such as vasculitis (44, 48), multiple sclerosis (8), and liver disease, including acute and chronic hepatitis (36, 47). Moreover, sCD14 has been shown to down-regulate lymphocyte activation and function (37), and its action, combined with that of IL-10 and with substantial reductions in viral Ag levels, may play a role in diminishing liver damage during IFN-α therapy. Our finding of increased circulating IL-10 levels during IFN-α treatment is consistent with the findings presented in a previous report by Aman et al. (2), who showed that IFN-α enhances IL-10 production by peripheral blood mononuclear cells in vitro. They were able to detect this phenomenon in purified monocyte and CD4+-T-cell populations only in conjunction with stimulation with LPS and mitogen, respectively. Increased levels of CD14 expression on Kupffer cells may have also contributed to the enhancement of circulating IL-10, since it is known that the physiological concentrations of LPS reaching the liver through the portal vein induce continuous IL-10 production by Kupffer cells (22).
In conclusion, the present study suggests that therapy with IFN-α reduces liver inflammation in patients with CHB. The presence in the liver of CD14+ macrophages capable of enhanced removal of antigenic material reduces T-cell activation and the potentially harmful recruitment of bystander lymphocytes. At the systemic level, increased levels of circulating sCD14 and IL-10, both of which are known to be down-modulators of lymphocytic activation, contribute further to this anti-inflammatory activity.
Acknowledgments
We are indebted to Marjan van Meurs and Luc Nelemans for helpful technical assistance; and we thank the staff of the Molecular Biology Diagnostic section of the Department of Virology, Erasmus Medical Center, for HBV DNA load assessment.
This work was supported by a grant from the European Commission (Biotech 2).
REFERENCES
- 1.Albert, M. L., S. F. A. Pearce, L. M. Francisco, B. Sauter, P. Roy, R. L. Silverstein, and N. Bhardwaj. 1998. Immature dendritic cells phagocytose apoptotic cells via alpha(v)beta(5) and CD36, and cross-present antigens to cytotoxic T lymphocytes. J. Exp. Med. 188:1359-1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aman, M. J., T. Tretter, I. Eisenbeis, G. Bug, T. Decker, W. E. Aulitzky, H. Tilg, C. Huber, and C. Peschel. 1996. Interferon-α stimulates production of interleukin-10 in activated CD4+ cells and monocytes. Blood 87:4731-4736. [PubMed] [Google Scholar]
- 3.Barron, M. A., N. Blyveis, B. E. Palmer, S. MaWhinney, and C. C. Wilson. 2003. Influence of plasma viremia on defects in number and immunophenotype of blood dendritic cell subsets in human immunodeficiency virus 1-infected individuals. J. Infect. Dis. 187:26-37. [DOI] [PubMed] [Google Scholar]
- 4.Belardelli, F., and I. Gresser. 1996. The neglected role of type I interferon in the T-cell response: implications for its clinical use. Immunol. Today 17:369-372. [DOI] [PubMed] [Google Scholar]
- 5.Bertoletti, A., M. Maini, and R. Williams. 2003. Role of hepatitis B virus specific cytotoxic T cells in liver damage and viral control. Antivir. Res. 60:61-66. [DOI] [PubMed] [Google Scholar]
- 6.Billiau, A. 1986. The mode of action of interferons in viral infections and their possible role in the control of hepatitis B. J. Hepatol. 3(Suppl. 2):S171-S179. [DOI] [PubMed] [Google Scholar]
- 7.Brassard, D. L., M. J. Grace, and R. W. Bordens. 2002. Interferon-α as an immunotherapeutic protein. J. Leukoc. Biol. 71:565-581. [PubMed] [Google Scholar]
- 8.Brettschneider, J., D. Ecker, A. Bitsche, D. Bahner, T. Bogumil, A. Dressel, E. Elitok, B. Kitze, S. Poser, F. Weber, and H. Tumani. 2002. The macrophage activity marker sCD14 is increased in patients with multiple sclerosis and upregulated by interferon beta-1b. J. Neuroimmunol. 133:193-197. [DOI] [PubMed] [Google Scholar]
- 9.Der, S. D., A. Zhou, B. R. G. Williams, and R. H. Silverman. 1998. Identification of genes differentially regulated by interferon alpha, beta, or gamma using oligonucleotide array. Proc. Natl. Acad. Sci. USA 95:15623-15628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Devitt, A., O. D. Moffatt, C. Raykundalia, J. D. Capra, D. L. Simmons, and C. D. Gregory. 1998. Human CD14 mediates recognition and phagocytosis of apoptotic cells. Nature 392:505-509. [DOI] [PubMed] [Google Scholar]
- 11.Dziarski, R., R. I. Tapping, and P. S. Tobias. 1998. Binding of bacterial peptidoglycan to CD14. J. Biol. Chem. 273:8680-8690. [DOI] [PubMed] [Google Scholar]
- 12.Egle, A., A. Villunger, M. Kos, G. Bock, J. Gruber, B. Auer, and R. Greil. 1996. Modulation of Apo-1/Fas (CD95)-induced programmed cell death in myeloma cells by interferon-α2. Eur. J. Immunol. 26:3119-3126. [DOI] [PubMed] [Google Scholar]
- 13.Erickson, S., O. Sangfelt, J. Castro, M. Heyman, S. Einhorn, and D. Grander. 1999. Interferon-alpha inhibits proliferation in human T lymphocytes by abrogation of interleukin 2-induced changes in cell cycle-regulatory proteins. Cell Growth Differ. 10:575-582. [PubMed] [Google Scholar]
- 14.Fujihara, M., M. Muroi, K. Tanamoto, T. Suzuki, H. Azuma, and H. Ikeda. 2003. Molecular mechanisms of macrophage activation and deactivation by lipopolysaccharide: roles of the receptor complex. Pharmacol. Ther. 100:171-194. [DOI] [PubMed] [Google Scholar]
- 15.Gallucci, S., M. Lolkema, and P. Matzinger. 1999. Natural adjuvants: endogenous activators of dendritic cells. Nat. Med. 5:1249-1255. [DOI] [PubMed] [Google Scholar]
- 16.Goddard, G., J. Youster, E. Morgan, and D. H. Adams. 2004. Interleukin-10 secretion differentiates dendritic cells from human liver and skin. Am. J. Pathol. 164:511-519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gregory, C. D. 2000. CD14-dependent clearance of apoptotic cells: relevance to the immune system. Curr. Opin. Immunol. 12:27-34. [DOI] [PubMed] [Google Scholar]
- 18.Guidotti, L. G., and F. V. Chisari. 2001. Noncytolytic control of viral infections by the innate and adaptive immune response. Annu. Rev. Immunol. 19:65-91. [DOI] [PubMed] [Google Scholar]
- 19.Kadowaki, N., S. Antonenko, J. Y. Lau, and Y. J. Liu. 2000. Natural interferon alpha/beta-producing cells link innate and adaptive immunity. J. Exp. Med. 192:219-226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kirou, K. A., R. K. Vakkalanka, M. J. Butler, and M. K. Crow. 2000. Induction of Fas ligand-mediated apoptosis by interferon-alpha. Clin. Immunol. 95:218-226. [DOI] [PubMed] [Google Scholar]
- 21.Kitchens, R. L., P. A. Thompson, S. Viriyakosol, G. E. O'Keefe, and R. S. Munford. 2001. Plasma CD14 decreases monocyte responses to LPS by transferring cell-bound LPS to plasma lipoproteins. J. Clin. Investig. 108:485-493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Knolle, P., J. Schlaak, A. Uhrig, P. Kempf, K. H. Meyer zum Buschenfelde, and G. Gerken. 1995. Human Kupffer cells secrete IL10 in response to lipopolysaccharide (LPS) challenge. J. Hepatol. 22:226-229. [DOI] [PubMed] [Google Scholar]
- 23.Knolle, P. A., and G. Gerken. 2000. Local control of the immune response in the liver. Immunol. Rev. 174:21-34. [DOI] [PubMed] [Google Scholar]
- 24.Kudo, S., K. Matsuno, T. Ezaki, and M. Ogawa. 1997. A novel migration pathway for rat dendritic cells from blood: hepatic sinusoids-lymph translocation. J. Exp. Med. 185:777-784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kunitani, H., Y. Shimizu, H. Murata, K. Higuchi, and A. Watanabe. 2002. Phenotypic analysis of circulating and intrahepatic dendritic cell subsets in patients with chronic liver diseases. J. Hepatol. 36:734-741. [DOI] [PubMed] [Google Scholar]
- 26.Kurt-Jones, E. A., L. Popova, L. Kwinn, L. M. Haynes, L. P. Jones, R. A. Tripp, E. E. Walsh, M. W. Freeman, D. T. Golenbock, L. J. Anderson, and R. W. Finberg. 2000. Pattern recognition receptors TLR4 and CD14 mediate response to respiratory syncytial virus. Nat. Immunol. 1:398-401. [DOI] [PubMed] [Google Scholar]
- 27.Lai, C. L., R. N. Chien, N. W. Leung, T. T. Chang, R. Guan, D. I. Tai, K. J. Ng, P. C. Wu, J. C. Dent, J. Barber, S. L. Stephenson, and D. F. Gray. 1998. A one-year trial of lamivudine for chronic hepatitis B. N. Engl. J. Med. 339:61-68. [DOI] [PubMed] [Google Scholar]
- 28.Li, C., S. Chi, N. He, X. Zhang, O. Guicherit, R. Wagner, S. Tyring, and J. Xie. 2004. IFN-alpha induces Fas expression and apoptosis in hedgehog pathway activated BCC cells through inhibiting Ras-Erk signaling. Oncogene 23:1608-1617. [DOI] [PubMed] [Google Scholar]
- 29.Limmer, A., J. Ohl, C. Kurts, H. G. Ljunggren, Y. Reiss, M. Groettrup, F. Momburg, B. Arnold, and P. A. Knolle. 2000. Efficient presentation of exogenous antigen by liver endothelial cells to CD8+ T cells results in antigen-specific T cell tolerance. Nat. Med. 6:1348-1354. [DOI] [PubMed] [Google Scholar]
- 30.Liu, S., L. S. Khemlani, R. A. Shapiro, M. L. Johnson, K. Liu, D. A. Geller, S. C. Watkins, S. M. Goyert, and T. R. Billiar. 1998. Expression of CD14 by hepatocytes: upregulation by cytokine during endotoxemia. Infect. Immun. 66:5089-5098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Luft, T., K. C. Pang, E. Thomas, C. J. Bradley, H. Savoia, J. Trapani, and J. Cebon. 1998. Type I IFNs enhance the terminal differentiation of dendritic cells. J. Immunol. 161:1947-1953. [PubMed] [Google Scholar]
- 32.Maini, M. K., C. Boni, C. K. Lee, J. R. Larrubia, S. Reignat, G. S. Ogg, A. S. King, J. Herberg, R. Gilson, A. Alisa, R. Williams, D. Vergani, N. V. Naoumov, C. Ferrari, and A. Bertoletti. 2000. The role of virus-specific CD8+ cells in liver damage and viral control during persistent hepatitis B virus infection. J. Exp. Med. 191:1269-1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Matsuura, K., T. Ishida, M. Setoguchi, Y. Higuchi, S. Akizuki, and S. Yamamoto. 1994. Upregulation of mouse CD14 expression in Kupffer cells by lipopolysaccharide. J. Exp. Med. 179:1671-1676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Niederau, C., T. Heintges, S. Lange, G. Goldmann, C. M. Niederau, L. Mohr, and D. Haussinger. 1996. Long-term follow-up of HBeAg-positive patients treated with interferon-alpha for chronic hepatitis B. N. Engl. J. Med. 334:1422-1427. [DOI] [PubMed] [Google Scholar]
- 35.Niesters, H. G., M. Krajden, L. Cork, M. de Medina, M. Hill, E. Fries, and A. D. Osterhaus. 2000. A multicenter study evaluation of the Digene Hybrid Capture II signal amplification technique for detection of hepatitis B virus DNA in serum samples and testing of EUROHEP standards. J. Clin. Microbiol. 38:2150-2155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Oesterreicher, C., F. Pfeffel, D. Petermann, and C. Muller. 1995. Increased in vitro production and serum levels of the soluble lipopolysaccharide receptor CD14 in liver disease. J. Hepatol. 23:396-402. [DOI] [PubMed] [Google Scholar]
- 37.Rey Nores, J. E., A. Bensussan, N. Vita, F. Stelter, M. A. Arias, M. Jones, S. Lefort, L. K. Borysiewicz, P. Ferrara, and M. O. Labeta. 1999. Soluble CD14 acts as a negative regulator of human T cell activation and function. Eur. J. Immunol. 29:256-276. [DOI] [PubMed] [Google Scholar]
- 38.Riffault, S., C. Carrat, L. Besnarderau, B. La Bonnadiere, and B. Charley. 1997. In vivo induction of interferon-alpha in pig by non-infectious coronavirus: tissue localization and in situ phenotypic characterization of interferon-alpha producing cells. J. Gen. Virol. 78:2483-2487. [DOI] [PubMed] [Google Scholar]
- 39.Romani, N., D. Reider, M. Heuer, S. Ebner, E. Kampgen, B. Eibl, D. Niederwieser, and G. Schuler. 1996. Generation of mature dendritic cells from human blood. An improved method with special regard to clinical applicability. J. Immunol. Methods 196:137-151. [DOI] [PubMed] [Google Scholar]
- 40.Sallusto, F., and A. Lanzavecchia. 1994. Efficient presentation of soluble antigen by cultured human dendritic cells is maintained by granulocyte/macrophage colony-stimulating factor plus interleukin 4 and downregulated by tumor necrosis factor alpha. J. Exp. Med. 179:1109-1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Samuel, C. E. 2001. Antiviral actions of interferons. Clin. Microbiol. Rev. 14:778-809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sanceau, J., D. D. Boyd, M. Seiki, and B. Bauvois. 2002. Interferons inhibit tumor necrosis factor-α-mediated matrix metalloproteinase-9 activation via interferon regulatory factor-1 binding competition with NF-κB. J. Biol. Chem. 277:35766-35775. [DOI] [PubMed] [Google Scholar]
- 43.Santini, S. M., C. Lapenta, M. Logozzi, S. Parlato, M. Spada, T. Di Pucchio, and F. Belardelli. 2000. Type I interferon as a powerful adjuvant for monocyte-derived dendritic cell development and activity in vitro and in Hu-PBL-SCID mice. J. Exp. Med. 191:1777-1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Scherberic, J. F., and W. A. Nockher. 1999. CD14++ monocytes, CD14+/CD16+ subset and soluble CD14 as biological markers of inflammatory systemic disease and monitoring immunosuppressive therapy. Clin. Chem. Lab. Med. 37:209-213. [DOI] [PubMed] [Google Scholar]
- 45.Selleri, C., T. Sato, L. Del Vecchio, L. Luciano, A. J. Barrett, B. Rotoli, N. S. Young, and J. P. Maciejewski. 1997. Involvement of Fas-mediated apoptosis in the inhibitory effect of interferon-α in chronic myelogenous leukemia. Blood 89:957-964. [PubMed] [Google Scholar]
- 46.Sitia, G., M. Isogawa, M. Iannacone, I. L. Campbell, F. V. Chisari, and L. G. Guidotti. 2004. MMPs are required for recruitment of antigen non-specific mononuclear cells into the liver by CTLs. J. Clin. Investig. 113:1158-1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Steyaert, S., P. Vanlandschoot, H. van Vlierberghe, H. Diepolder, and G. Leroux-Roels. 2003. Soluble CD14 levels are increased and inversely correlated with the levels of hepatitis B surface antigen in chronic hepatitis B patients. J. Med. Virol. 71:188-194. [DOI] [PubMed] [Google Scholar]
- 48.Takeshita, S., K. Nakatani, H. Tsujimoto, Y. Kawamura, H. Kawase, and I. Sekine. 2000. Increased levels of circulating soluble CD14 in Kawasaki disease. Clin. Exp. Immunol. 19:376-381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Thomson, A. W., and L. Lu. 1999. Are dendritic cells the key to liver transplant tolerance? Immunol. Today 20:27-32. [DOI] [PubMed] [Google Scholar]
- 50.Tomita, M., K. Yamamoto, H. Kobashi, M. Ohmoto, and T. Tsuji. 1994. Immunohistochemical phenotyping of liver macrophages in normal and diseased human liver. Hepatology 20:317-325. [PubMed] [Google Scholar]
- 51.Zhou, L. J., and T. F. Tedder. 1995. Human blood dendritic cells selectively express CD83, a member of the immunoglobulin superfamily. J. Immunol. 154:3821-3835. [PubMed] [Google Scholar]