Abstract
Background:
Tyrosine kinase inhibitors (TKIs) are associated with prolongation of the QTc interval on the electrocardiogram (ECG). The QTc-interval prolongation increases the risk of life-threatening arrhythmias. However, studies evaluating the effects of TKIs on QTc intervals are limited and only consist of small patient numbers.
Methods:
In this multicentre trial in four centres in the Netherlands and Italy we screened all patients who were treated with any TKI. To evaluate the effects of TKIs on the QTc interval, we investigated ECGs before and during treatment with erlotinib, gefitinib, imatinib, lapatinib, pazopanib, sorafenib, sunitinib, or vemurafenib.
Results:
A total of 363 patients were eligible for the analyses. At baseline measurement, QTc intervals were significantly longer in females than in males (QTcfemales=404 ms vs QTcmales=399 ms, P=0.027). A statistically significant increase was observed for the individual TKIs sunitinib, vemurafenib, sorafenib, imatinib, and erlotinib, after the start of treatment (median ΔQTc ranging from +7 to +24 ms, P<0.004). The CTCAE grade for QTc intervals significantly increased after start of treatment (P=0.0003). Especially patients who are treated with vemurafenib are at increased risk of developing a QTc of ⩾470 ms, a threshold associated with an increased risk for arrhythmias.
Conclusions:
These observations show that most TKIs significantly increase the QTc interval. Particularly in vemurafenib-treated patients, the incidence of patients at risk for arrhythmias is increased. Therefore, especially in case of combined risk factors, ECG monitoring in patients treated with TKIs is strongly recommended.
Keywords: tyrosine kinase inhibitors, QTc interval, arrhythmia, ECG
Long QT syndrome (LQTS) is a myocardial repolarisation disorder characterised by prolongation of the QT interval on the surface electrocardiogram (ECG). The clinical presentation of LQTS consists of palpitations, syncope, seizures, and sudden cardiac death due to a characteristic arrhythmia known as torsades de pointes (TdP) (El-Sherif and Turitto, 2003; Moss, 2003; Trinkley et al, 2013).
The QT interval represents the total duration of ventricular depolarisation and repolarisation. It is measured on the ECG from the first deflection of the QRS complex to the end of the T-wave. Prolongation of the QT interval usually results from delayed repolarisation. This can be caused by drugs or inherited ion channel abnormalities, which block or result in loss of function of potassium channels (IKr, IKs, and IKl), or opening or gain of function of sodium (Ina) or calcium channels (Grant, 2009). The QT interval is usually corrected for heart rate, leading to the corrected QT interval QTc.
Several factors such as gender, age, electrolyte disturbances, cardiovascular diseases (CVD), and different types of drugs can affect the duration of the QT interval (Yetkin et al, 2001; Benoit et al, 2005). Due to the risk of fatal arrhythmias, the US Food and Drug Administration (FDA) now requires thorough studies to evaluate the potency of new drugs to induce QT-interval prolongation in preclinical and early phase I clinical trials in healthy individuals (El-Sherif and Turitto, 2003). However, for new anticancer drugs these studies are usually not performed in healthy individuals because of their toxicity profile (Curigliano et al, 2008; de Jonge and Verweij, 2008).
As with many drugs, tyrosine kinase inhibitors (TKIs) are reported to prolong the QT interval (Strevel et al, 2007; Bello et al, 2009; Lee et al, 2010; Tolcher et al, 2011; Dogan et al, 2012; Doherty et al, 2013; Dong et al, 2013; Heath et al, 2013; Shah et al, 2013). In vitro studies demonstrated that lapatinib and imatinib interact with the phosphorylation of the cardiac hERG channel. This results in a reduction of the repolarising current (IKr), which can lead to action potential prolongation and subsequent QT-interval prolongation (Lee et al, 2010; Dong et al, 2013).
In a small prospective clinical study to evaluate the cardiac safety of lapatinib in 21 patients, a mean QTc increase of 8.63 ms was seen (Dogan et al, 2012). In three prospective post-marketing studies in patients with solid tumours treated with sorafenib (N=31), pazopanib (N=48), and sunitinib (N=24) a modest increase of 9.0 ms of QTc interval with the use of sorafenib, 4.4 ms after start of pazopanib and 9.6 ms after start of sunitinib was seen (Bello et al, 2009; Tolcher et al, 2011; Heath et al, 2013).
These drugs have been approved by the FDA because they appear highly effective in situations where treatment options are limited. With an increasing number of TKIs on market, a relatively long on-treatment time, and the application in the adjuvant setting, which is already standard for imatinib in patients with localised GIST with a high risk of relapse, and which is being explored for other TKIs in various tumour types, thorough QTc studies in this group of drugs are necessary to get more insight into their cardiac safety. In this multicentre study performed in four centres in the Netherlands and Italy, we describe the incidence and relevance of QTc-interval prolongation in patients with cancer treated with different types of TKIs.
Patients and methods
Study design
We undertook a retrospective study in patients with solid malignancies, who were treated with any type of TKI. Patients from four centres in the Netherlands (Erasmus MC Cancer Institute, Rotterdam, Leiden University Medical Centre, Leiden, and Netherlands Cancer Institute—Antoni van Leeuwenhoek, Amsterdam) and Italy (Salvatore Maugeri Foundation, Pavia) were included.
This study was reviewed and approved by the Erasmus MC Medical Ethical Board (MEC 2013-148). All ECGs were obtained as standard clinical care. Demographic and clinical characteristics of the analysed cohort were collected using clinical record forms designed for this study.
Patients were considered eligible if they were aged ⩾18 years, were treated for solid tumours with any type of TKI and if at least one ECG before start of TKI treatment and one ECG during treatment with TKI were available. Exclusion criteria were as follows: ECGs that do not match criteria for accurate QTc-interval measurements (intra-ventricular conduction delay and/or pacemaker driven rhythm), missing ECGs at baseline or during therapy, and patients with a time-lapse between baseline ECG and start of TKI treatment of more than 1 year. Patients who were subsequently treated with different TKIs were included once. All standard 12-lead ECGs analysed in this study were reviewed by a single expert cardiologist (CN). The QT interval was measured from the beginning of the QRS complex until the point where the deflection of the T wave crosses the iso-electric line. A description of the statistical method is presented in the Supplementary Material.
Definition of QTc prolongation
Since increases in heart rate result in shortening of the QT interval, a correction for heart rate was applied using the Bazett formula (Sagie et al, 1992):
 |
In this formula, RR is the interval between two subsequent R waves. The Bazett formula is the most frequently applied correction in clinical practice, leading to the corrected QT interval or QTc interval (Sagie et al, 1992).
A prolonged QT interval is associated with an increased risk of polymorphic ventricular tachycardia, torsade de pointes (TdP). This study defined a prolonged QT interval corrected for heart rate (QTc) as ⩾470 ms, which represents <0.5% of the healthy population (Kobza et al, 2009) and has been shown to be associated with an increased risk of TdP (Trinkley et al, 2013). A clinically relevant increase in QTc (ΔQTc) was defined as an increase of ⩾30 ms between a patient's baseline and subsequent ECG as this has also been shown to be associated with increased risk (Li et al, 2010). The QTc was also categorised according to the Common terminology criteria for adverse events (CTCAE) guidelines version 4.03 (grade 0, QTc<450; grade 1, QTc 450–479 ms; grade 2, QTc 480–499 ms; grade 3, QTc⩾500 ms; grade 4, QTc⩾500 ms with life-threatening signs or symptoms; grade 5, death). Relevant CVD was defined as myocardial infarction and/or heart failure.
Outcome measures used in this study were (i) the quantitative difference in QTc interval between on therapy and baseline ECG measurements (ΔQTc, ms), (ii) the transition from a condition of normal repolarisation to a condition in which QTc is prolonged to an extent with high risk of arrhythmia as a consequence of the TKI therapy (i.e., from QTc<470 to QTc⩾470 ms) (Kobza et al, 2009; Trinkley et al, 2013), (iii) clinically relevant ΔQTc (defined as ΔQTc⩾30 ms, above which the risk for TdP is significantly increased) (Li et al, 2010) and (iv) QTc-interval CTCAE grade increase during TKI therapy.
Results
Patient characteristics
A total of 1933 cases of TKI use were screened in this study. In 644 cases at least one ECG before treatment and one ECG during treatment were available. Among these cases, 18 patients were included twice, with subsequent use of different TKIs. One patient had a pacemaker-driven rhythm. In 262 patients, the time lapse between baseline ECG and start of treatment was more than 1 year and patients were therefore excluded from the analysis. The remaining study cohort consisted of 363 patients. The median age at start of treatment was 60 years (interquartile range (IQR) 51–67), and 59% of patients were male. Sunitinib was the most frequently used TKI in our study cohort, with a total of 110 treated patients. The median QTc interval at baseline visit was 401 ms (IQR 388–415), where 346 patients (95.3%) had a normal QTc interval (CTCAE grade 0), 14 (3.9%) had grade 1, 2 patients (0.6%) had grade 2, and 1 patient (0.3%) had a grade 3 QTc interval. A total number of 37 patients (10.2%) had a known history of relevant CVD, while 34 patients (9.4%) used co-medication, that can lead to QTc-interval prolongation (Strevel et al, 2007). Patients' demographics and disease characteristics are presented in Table 1.
Table 1. Patient characteristics.
| Variable | N (%) or median (IQR) |
|---|---|
|
Gender | |
| Male | 215 (59) |
| Female | 148 (41) |
| Age (years) | 60 (51–67) |
| QTc-interval baseline | 401 (388–415) |
| QTc-interval therapy | 415 (397–431) |
|
Tumour type | |
| RCC | 101 (27.8) |
| GIST | 49 (13.5) |
| HCC | 45 (12.4) |
| Lung cancer | 27 (7.4) |
| Breast cancer | 16 (4.4) |
| Melanoma | 69 (19.0) |
| Other | 56 (15.4) |
|
Type of TKI | |
| Sunitinib | 110 (30.3) |
| Vemurafenib | 67 (18.5) |
| Sorafenib | 52 (14.3) |
| Pazopanib | 46 (12.7) |
| Imatinib | 41 (11.3) |
| Erlotinib | 21 (5.8) |
| Lapatinib | 16 (4.4) |
| Gefitinib | 10 (2.8) |
|
WHO PS baseline | |
| 0 | 155 (42.7) |
| 1 | 195 (53.7) |
| 2 | 12 (3.3) |
| 3 | 1 (0.3) |
| CVD | 37 (10.2) |
| QTc co-medications | 34 (9.4) |
|
Race | |
| Caucasian | 349 (96.1) |
| Other | 14 (3.5) |
|
Site | |
| EMC | 184 (50.7) |
| NKI | 118 (32.5) |
| LUMC | 54 (14.9) |
| SMF | 7 (1.9) |
Abbreviations: CVD=cardiovascular disease; EMC=Erasmus MC—Cancer Institute; GIST=gastro-intestinal stromal tumour; HCC=hepatocellular carcinoma; LUMC=Leiden University Medical Centre; NKI=Netherlands Cancer Institute—Antoni van Leeuwenhoek; RCC=renal cell cancer; SMF=Salvatore Maugeri Foundation; TKI=tyrosine kinase inhibitor; WHO PS=World Health Organisation performance score.
Variables modulating QTc interval at baseline visit
At baseline measurements, QTc was slightly, but significantly greater in females than in males (QTcfemales=404 ms (IQR 392–417) vs QTcmales=399 ms (IQR 385–414), P=0.027), which is consistent with previous studies (Strevel et al, 2007). Patients treated with co-medication known to prolong the QTc interval, such as anti-depressants, anti-epileptics, and anti-emetics, had a statistically significant higher baseline QTc interval than the patients who did not use such co-medication (409 ms (IQR 398–424) vs 400 ms (IQR 387–414), respectively, P=0.035). Consistent with previous studies, patients suffering from hypokalaemia had longer median QTc intervals than patients with normokalaemia and hyperkalaemia (median QTc in hypokalaemic, normokalaemic, and hyperkalaemic patients 416 ms (IQR 376–431), 401 ms (IQR 389–415), and 391 ms (IQR 381–408), P=0.028, respectively). A more detailed report about baseline QTc intervals according to the evaluated variables is found in Supplementary Table 1.
Quantitative variations of the QTc interval
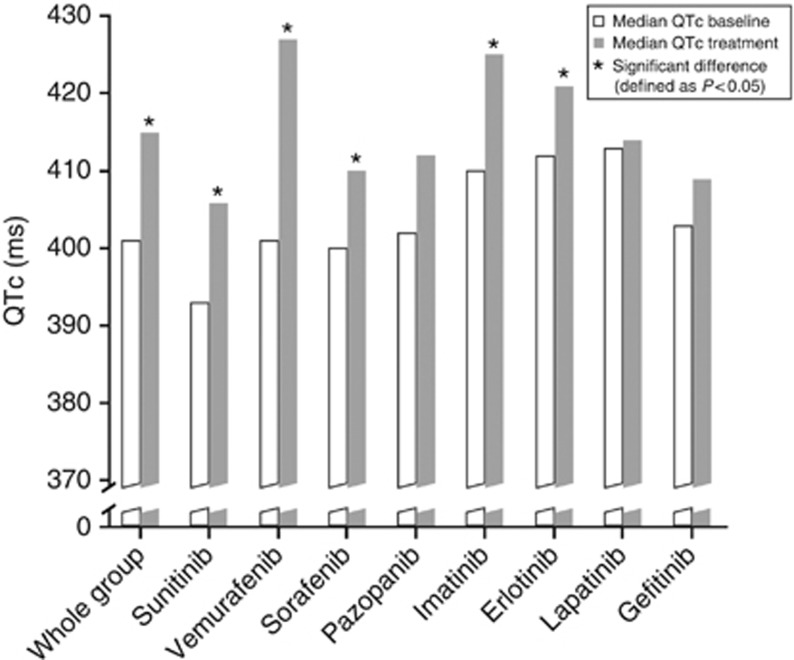
The median on treatment time before the ECG was performed was 43 days (IQR 26–118 days). In the entire population of 363 patients, the start of a TKI resulted in a statistically significant increase in QTc interval, with a median ΔQTc of +11 ms (P<0.00001). The distribution of ΔQTc was significantly different across TKIs (P=0.0001). When analysing subgroups of patients treated with specific TKIs, patients treated with sunitinib (N=110), vemurafenib (N=67), sorafenib (N=52), imatinib (N=41), and erlotinib (N=21) showed a statistically significant increase in QTc interval after start of treatment (median ΔQTc ranging from +7 to +24 ms, P<0.004; Figure 1). For lapatinib (N=16) and pazopanib (N=46), no statistically significant increase in QTc interval after start of treatment was found (Table 2).
Figure 1.
ΔQTc in the whole cohort and in specific TKIs. Blue bars represent the median baseline QTc interval and red bars represent the median QTc interval during treatment. At the y axis, the QTc interval is expressed in ms.
Table 2. TKI-induced change in QTc interval.
|
QTc interval (ms)
Median (IQR) |
||||
|---|---|---|---|---|
| TKI | n | Baseline | Therapy | P-value |
| Whole | 363 | 401 (388–415) | 415 (397–431) | <0.00001 |
| Sunitinib | 110 | 393 (380–410) | 406 (390–424) | <0.00001 |
| Vemurafenib | 67 | 401 (394–417) | 427 (415–442) | <0.00001 |
| Sorafenib | 52 | 400 (386–412) | 410 (394–425) | 0.0004 |
| Pazopanib | 46 | 402 (390–411) | 412 (395–431) | 0.079 |
| Imatinib | 41 | 410 (396–424) | 425 (410–439) | 0.002 |
| Erlotinib | 21 | 412 (398–430) | 421 (414–440) | 0.004 |
| Lapatinib | 16 | 413 (405–423) | 414 (397–428) | 0.982 |
| Gefitinib | 10 | 403 (396–417) | 409 (390–429) | 0.919 |
Abbreviations: IQR=interquartile range; n=number of patients within each TKI group; ΔQTc=median difference between QTc interval during TKI treatment and QTc interval at baseline; TKI=tyrosine kinase inhibitor. Bold values are statistically significant.
Increase in CTCAE grade and prevalence of high-risk patients
A statistically significant increase in CTCAE grade for QTc intervals was observed after start of TKI therapy in the whole cohort (P=0.0003). In detail, 33 patients (9.1%) were characterised by an increased CTCAE grade. Of these, 31 passed from grade 0 to grade⩾1, while the remaining 2 individuals passed from grade 1 to grade 2 or 3. Of the remaining patients, 321 (88.4%) did not have an increase or decrease in CTCAE grade after start of TKI treatment, while 9 patients (2.5%) had a reduced CTCAE grade for QTc interval (Table 3).
Table 3. Increase in CTCAE grade and prevalence of high-risk patients.
|
Change in CTCAE Grade after start of therapy |
QTc⩾470 |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| TKI | N | ΔQTc⩾30 ms N (%) | Increased N (%) | Unchanged N (%) | Reduced N (%) | P-value | Baseline N (%) | Therapy N (%) | P-value |
| Whole | 363 | 76 (20.9) | 33 (9.1) | 321 (88.4) | 9 (2.5) | 0.0003 | 6 (1.7) | 21 (5.8) | 0.005 |
| Sunitinib | 110 | 22 (20.0) | 4 (3.6) | 104 (95.6) | 2 (1.8) | 0.746 | 1 (0.9) | 3 (2.7) | 0.617 |
| Vemurafenib | 67 | 23 (34.3) | 9 (13.4) | 58 (86.6) | 0 (0) | 0.008 | 1 (1.5) | 8 (11.9) | 0.023 |
| Sorafenib | 52 | 11 (21.2) | 6 (11.6) | 45 (86.6) | 1 (1.9) | 0.073 | 1 (1.9) | 2 (3.9) | 1 |
| Pazopanib | 46 | 6 (13.0) | 3 (6.5) | 41 (89.1) | 2 (4.4) | 0.410 | 1 (2.2) | 2 (4.4) | 1 |
| Imatinib | 41 | 8 (19.5) | 5 (12.2) | 34 (82.9) | 2 (4.9) | 0.430 | 1 (2.4) | 1 (2.4) | 1 |
| Erlotinib | 21 | 3 (14.3) | 3 (14.3) | 18 (85.7) | 0 (0) | 0.174 | 0 (0) | 2 (9.5) | NA |
| Lapatinib | 16 | 1 (6.3) | 1 (6.3) | 14 (87.5) | 1 (6.3) | 1 | 1 (6.3) | 1 (6.3) | 1 |
| Gefitinib | 10 | 2 (20.0) | 2 (20.0) | 7 (70.0) | 1 (10.0) | 0.423 | 0 (0) | 2 (20.0) | NA |
Abbreviations: CTCAE=common terminology criteria for adverse events; N=number of patients; NA=not applicable; TKI=tyrosine kinase inhibitor; ΔQTc=difference between QTc interval during TKI treatment and QTc interval at baseline measurement. Bold values are statistically significant.
Similarly, a statistically significant increase in the prevalence of high-risk patients was observed after TKI therapy start (QTcbaseline⩾470 ms=1.7% vs QTctherapy⩾470 ms=5.8%, P=0.005), with 20 individuals (5.5%) who transitioned from a low-risk to a high-risk condition. Moreover, 5 patients (1.4%) developed QTc⩾500 ms (CTCAE grade 3) after therapy start, and 76 patients (20.9%) experienced a clinically relevant QTc increase after TKI start. All five patients who developed QTc⩾500 ms after start of therapy had a ΔQTc of ⩾100 ms.
When focusing on specific TKI subgroups, we observed that individuals treated with vemurafenib (N=67) were characterised by a statistically significant increase both in terms of CTCAE grade for QTc intervals (P=0.008) and in the probability of becoming high-risk patients (P=0.023), also showing the greatest probability of clinically relevant QTc increase (34.3%). No statistically significant variations in the evaluated outcomes were observed in the other TKI subgroups.
Characterisation of TKI-induced QTc variability
The median age of patients who had a worsening of the CTCAE grade for QTc interval was significantly higher than that of patients who did not (62 years (IQR 59–72) vs 60 years (IQR 51–67), respectively, P=0.023). These patients also more often suffered from hypokalaemia (20.7% vs 3.1%, P=0.0009; Table 4). Multivariate logistic regression confirmed that age and hypokalaemia were independent predictors of worsened CTCAE grade for QTc interval (OR=1.10, 95% CI=1.05–1.16, P=0.0002 and OR=10.30, 95% CI=2.22–4.64, P=0.002).
Table 4. Variables influencing CTCAE grade for QTc interval and the probability to become a high-risk patient.
|
CTCAE grade during TKI |
Transition to high risk (QTc⩾470 ms) |
||||||
|---|---|---|---|---|---|---|---|
| Variable | N | Increased (n=33) median (IQR) or N (%) | Unchanged/Reduced (n=330) median (IQR) or N (%) | P-value | Yes (n=20) median (IQR) or N (%) | No (n=343) median (IQR) or N (%) | P-value |
| Age (years) | 363 | 62 (59–72) | 60 (51–67) | 0.026 | 66 (60–76) | 60 (51–66) | 0.007 |
|
Gender | |||||||
| Males | 215 | 22 (66.7) | 193 (58.5) | 0.458 | 14 (70) | 201 (58.6) | 0.358 |
| Females | 148 | 11 (33.3) | 137 (41.5) | 6 (30) | 142 (41.4) | ||
|
Co-medication | |||||||
| Yes | 34 | 6 (18.2) | 28 (8.5) | 0.107 | 5 (25) | 29 (8.4) | 0.030 |
| No | 329 | 27 (81.8) | 302 (91.5) | 15 (75) | 314 (91.6) | ||
|
CVD | |||||||
| Yes | 37 | 5 (15.2) | 32 (9.7) | 0.360 | 4 (20) | 33 (9.6) | 0.134 |
| No | 326 | 28 (84.9) | 298 (90.3) | 16 (80) | 310 (90.4) | ||
|
DM | |||||||
| Yes | 43 | 3 (9.1) | 40 (12.1) | 0.782 | 1 (5) | 42 (12.2) | 0.489 |
| No | 320 | 30 (90.9) | 290 (87.9) | 19 (95) | 301 (87.8) | ||
|
Ca2+ | |||||||
| Normo/Hyper | 169 | 13 (61.9) | 156 (71.6) | 0.451 | 8 (80) | 161 (70.3) | 0.728 |
| Hypo | 70 | 8 (38.1) | 62 (28.4) | 2 (20) | 68 (29.7) | ||
|
K+ | |||||||
| Normo/Hyper | 304 | 23 (79.3) | 281 (96.9) | 0.0009 | 16 (88.9) | 288 (95.7) | 0.204 |
| Hypo | 15 | 6 (20.7) | 9 (3.1) | 2 (11.1) | 13 (4.3) | ||
Abbreviations: Ca2+=calcium level at time of QTc measurement during treatment; CVD=cardiovascular disease; CTCAE, common terminology criteria for adverse events; DM=diabetes mellitus; IQR, interquartile range; K+, potassium level at time of QTc measurement during treatment; N, number of analysed patients with non-missing values; TKI, tyrosine kinase inhibitor. Bold values are statistically significant.
Similarly, patients who had QTc prolongation to ⩾470 ms after start of TKI treatment were significantly older than patients who did not (66 years (IQR 60–76) and 60 years (IQR 51–66), respectively, P=0.007) and were more frequently treated with QTc-prolonging co-medication (25% vs 8.5%, P=0.030). This was confirmed by multivariate logistic regression (OR=1.10, 95% CI=1.04–1.15, P=0.0004 and OR=4.38, 95% CI=1.14–15.25, P=0.023).
We did not identify variables that have a statistically significant impact on quantitative ΔQTc or on the probability of clinically relevant ΔQTc (Supplementary Table 2).
Discussion
We found a significant increase in QTc intervals after start of treatment with sunitinib, vemurafenib, sorafenib, imatinib, and erlotinib. In most cases, the increase in QTc interval is only modest and under normal conditions not clinically relevant. However, in 76 of the 363 patients the start of TKI treatment resulted in a clinically relevant increase of the QTc interval of ⩾30 ms. The incidence of high-risk patients, defined as QTc⩾470 ms (Trinkley et al, 2013), increased during treatment with a TKI. Still, only the subgroup receiving vemurafenib showed a statistically significant increase in the number of patients with QTc>470 ms.
In the entire cohort, 21% of patients showed a clinically relevant increase in QTc of ⩾30 ms with TKI treatment, but as most had a normal baseline QTc interval, only 5% had a QTc of ⩾470 ms, which is associated with increased risk of arrhythmias. Although older patients, patients with low potassium and patients taking co-medication which can prolong the QTc interval are at higher risk of QTc-interval prolongation, it is still not possible to differentiate which patient is at risk at the start of treatment.
Therefore, treating physicians should anticipate this possible increase in QTc intervals and perform ECGs during treatment with TKI, and be aware of symptoms, such as palpitation, seizures, and collapse, which may be the result of drug-induced LQTS. In those diseases where alternative treatment is available, such as in metastatic renal cell carcinoma where sunitinib and pazopanib have equivalent efficacy (Motzer et al, 2013), consideration should be given to use a TKI with less QTc prolongation effects if the QTc is prolonged at baseline or develops during treatment.
Furthermore, many patients use co-medication during TKI treatment. As drugs of a broad variety are known for drug-induced QTc-interval prolongation, it is likely that patients use several drugs which can lead to QTc-interval prolongation and thereby intensifying the effect on the QTc interval. This was shown in this study, where 14 patients (4%) using such co-medication were more likely to develop QTc prolongation. In those cases, extra awareness may be necessary and switching to drugs that are not likely to have an effect on QTc interval should be considered.
This study has several limitations. This was a retrospective study in patients treated with cancer, and therefore in most cases ECGs were not performed at predefined times before, during, and after TKI therapy. Since fluctuations in QTc interval are frequent and may be caused by many factors (Yetkin et al, 2001; Benoit et al, 2005), this is a weakness of our study, and may have influenced outcome (Molnar et al, 1996). Also, only patients treated with a TKI were included and there was no control group given non-TKI treatment in which the variation in the QTc interval could be examined. Furthermore, there may be a bias in patient selection since patients with cardiac events may be more likely to have had ECGs performed. Patients who died from arrhythmia may not have been included in analyses when no ECGs were available. One patient taking a TKI in the study died suddenly. This did not occur in a hospital and no cause of death was reported so it is unknown whether this was related to QTc-interval prolongation. Possible effects from electrolyte disorders on the QTc interval may have been missed, because of missing data. However, we showed in a large group of patients treated with TKIs that there is an overall increase in QTc interval after start of treatment, which may possibly be harmful for patients treated with these drugs. Future prospective studies could improve the current knowledge about TKI-induced QTc prolongation.
Overall, we may conclude that most TKIs tend to cause an increase in QTc intervals. In some cases, this increase is clinically relevant, and therefore the QTc interval should be verified in patients before starting TKI treatment and during therapy. Monitoring QTc intervals during TKI treatment is particularly important in patients with a history of QTc-interval prolongation, in patients using co-medication which can prolong the QTc interval, in patients with electrolyte disorders, and in patients with pre-existing CVD. Furthermore, during treatment with TKIs physicians should be aware of clinical symptoms, which may be attributed to QTc-interval prolongation.
Footnotes
Supplementary Information accompanies this paper on British Journal of Cancer website (http://www.nature.com/bjc)
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License.
This study was presented at the 2014 ASCO Annual Meeting in Chicago, Illinois.
Supplementary Material
References
- Bello CL, Mulay M, Huang X, Patyna S, Dinolfo M, Levine S, Van Vugt A, Toh M, Baum C, Rosen L. Electrocardiographic characterization of the QTc interval in patients with advanced solid tumors: pharmacokinetic- pharmacodynamic evaluation of sunitinib. Clin Cancer Res. 2009;15:7045–7052. doi: 10.1158/1078-0432.CCR-09-1521. [DOI] [PubMed] [Google Scholar]
- Benoit SR, Mendelsohn AB, Nourjah P, Staffa JA, Graham DJ. Risk factors for prolonged QTc among US adults: Third National Health and Nutrition Examination Survey. Eur J Cardiovasc Prev Rehabil. 2005;12:363–368. doi: 10.1097/01.hjr.0000173110.21851.a9. [DOI] [PubMed] [Google Scholar]
- Committee for Proprietary Medicinal Products (CPMP) Points to consider: The Assessment of the Potential for QT Interval Prolongation by non-Cardiovascular Medicinal ProductsVol. 1997The European Agency for the Evaluation of Medicinal Products: London, UK [Google Scholar]
- Common Terminology Criteria for Adverse Events (CTCAE), Version 4.03 U.S. Department of Health and Human ServicesNational Institutes of Health, National Cancer Institute published 14 June 2010.
- Curigliano G, Spitaleri G, Fingert HJ, de Braud F, Sessa C, Loh E, Cipolla C, De Pas T, Goldhirsch A, Shah R. Drug-induced QTc interval prolongation: a proposal towards an efficient and safe anticancer drug development. Eur J Cancer. 2008;44:494–500. doi: 10.1016/j.ejca.2007.10.001. [DOI] [PubMed] [Google Scholar]
- de Jonge M, Verweij J. QTc prolongation and/or oncology drug development: who's in danger. Eur J Cancer. 2008;44:486–487. doi: 10.1016/j.ejca.2008.01.013. [DOI] [PubMed] [Google Scholar]
- Dogan E, Yorgun H, Petekkaya I, Ozer N, Altundag K, Ozisik Y. Evaluation of cardiac safety of lapatinib therapy for ErbB2-positive metastatic breast cancer: a single center experience. Med Oncol. 2012;29:3232–3239. doi: 10.1007/s12032-012-0253-5. [DOI] [PubMed] [Google Scholar]
- Doherty KR, Wappel RL, Talbert DR, Trusk PB, Moran DM, Kramer JW, Brown AM, Shell SA, Bacus S. Multi-parameter in vitro toxicity testing of crizotinib, sunitinib, erlotinib, and nilotinib in human cardiomyocytes. Toxicol Appl Pharmacol. 2013;272:245–255. doi: 10.1016/j.taap.2013.04.027. [DOI] [PubMed] [Google Scholar]
- Dong Q, Fu XX, Du LL, Zhao N, Xia CK, Yu KW, Cheng LX, Du YM. Blocking of the human ether-a-go-go-related gene channel by imatinib mesylate. Biol Pharm Bull. 2013;36:268–275. doi: 10.1248/bpb.b12-00778. [DOI] [PubMed] [Google Scholar]
- El-Sherif N, Turitto G. Torsade de pointes. Curr Opin Cardiol. 2003;18:6–13. doi: 10.1097/00001573-200301000-00002. [DOI] [PubMed] [Google Scholar]
- Grant AO. Cardiac ion channels. Circ Arrhythm Electrophysiol. 2009;2:185–194. doi: 10.1161/CIRCEP.108.789081. [DOI] [PubMed] [Google Scholar]
- Heath EI, Infante J, Lewis LD, Luu T, Stephenson J, Tan AR, Kasubhai S, LoRusso P, Ma B, Suttle AB, Kleha JF, Ball HA, Dar MM. A randomized, double-blind, placebo-controlled study to evaluate the effect of repeated oral doses of pazopanib on cardiac conduction in patients with solid tumors. Cancer Chemother Pharmacol. 2013;71:565–573. doi: 10.1007/s00280-012-2030-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobza R, Roos M, Niggli B, Abacherli R, Lupi GA, Frey F, Schmid JJ, Erne P. Prevalence of long and short QT in a young population of 41,767 predominantly male Swiss conscripts. Heart Rhythm. 2009;6:652–657. doi: 10.1016/j.hrthm.2009.01.009. [DOI] [PubMed] [Google Scholar]
- Lee HA, Kim EJ, Hyun SA, Park SG, Kim KS. Electrophysiological effects of the anti-cancer drug lapatinib on cardiac repolarization. Basic Clin Pharmacol Toxicol. 2010;107:614–618. doi: 10.1111/j.1742-7843.2010.00556.x. [DOI] [PubMed] [Google Scholar]
- Li EC, Esterly JS, Pohl S, Scott SD, McBride BF. Drug-induced QT-interval prolongation: considerations for clinicians. Pharmacotherapy. 2010;30:684–701. doi: 10.1592/phco.30.7.684. [DOI] [PubMed] [Google Scholar]
- Molnar J, Zhang F, Weiss J, Ehlert FA, Rosenthal JE. Diurnal pattern of QTc interval: how long is prolonged? Possible relation to circadian triggers of cardiovascular events. J Am Coll Cardiol. 1996;27:76–83. doi: 10.1016/0735-1097(95)00426-2. [DOI] [PubMed] [Google Scholar]
- Moss AJ. Long QT Syndrome. JAMA. 2003;289:2041–2044. doi: 10.1001/jama.289.16.2041. [DOI] [PubMed] [Google Scholar]
- Motzer RJ, Hutson TE, Cella D, Reeves J, Hawkins R, Guo J, Nathan P, Staehler M, de Souza P, Merchan JR, Boleti E, Fife K, Jin J, Jones R, Uemura H, De Giorgi U, Harmenberg U, Wang J, Sternberg CN, Deen K, McCann L, Hackshaw MD, Crescenzo R, Pandite LN, Choueiri TK. Pazopanib versus sunitinib in metastatic renal-cell carcinoma. N Engl J Med. 2013;369:722–731. doi: 10.1056/NEJMoa1303989. [DOI] [PubMed] [Google Scholar]
- Sagie A, Larson MG, Goldberg RJ, Bengtson JR, Levy D. An improved method for adjusting the QT interval for heart rate (the Framingham Heart Study) Am J Cardiol. 1992;70:797–801. doi: 10.1016/0002-9149(92)90562-d. [DOI] [PubMed] [Google Scholar]
- Shah RR, Morganroth J, Shah DR. Cardiovascular safety of tyrosine kinase inhibitors: with a special focus on cardiac repolarisation (QT interval) Drug Saf. 2013;36:295–316. doi: 10.1007/s40264-013-0047-5. [DOI] [PubMed] [Google Scholar]
- Strevel EL, Ing DJ, Siu LL. Molecularly targeted oncology therapeutics and prolongation of the QT interval. J Clin Oncol. 2007;25:3362–3371. doi: 10.1200/JCO.2006.09.6925. [DOI] [PubMed] [Google Scholar]
- Tolcher AW, Appleman LJ, Shapiro GI, Mita AC, Cihon F, Mazzu A, Sundaresan PR. A phase I open-label study evaluating the cardiovascular safety of sorafenib in patients with advanced cancer. Cancer Chemother Pharmacol. 2011;67:751–764. doi: 10.1007/s00280-010-1372-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trinkley KE, Page RL, 2nd, Lien H, Yamanouye K, Tisdale JE. QT interval prolongation and the risk of torsades de pointes: essentials for clinicians. Curr Med Res Opin. 2013;29:1719–1726. doi: 10.1185/03007995.2013.840568. [DOI] [PubMed] [Google Scholar]
- Yetkin E, Senen K, Ileri M, Atak R, Topaloglu S, Ergun K, Yanik A, Tandogan I, Cehreli S, Duru E, Demirkan D. Diurnal variation of QT dispersion in patients with and without coronary artery disease. Angiology. 2001;52:311–316. doi: 10.1177/000331970105200503. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.